Epidemiologist Professor Jodie McVernon was in the Qantas lounge at Canberra airport on the evening of Monday, February 3, when she took an urgent call from Brendan Murphy, then the Commonwealth’s chief medical officer.
McVernon had for days been “obsessively” tracking information on the mysterious new virus seeping out of Wuhan, China, and was preparing to fly home to Melbourne after lengthy meetings in the national capital. But Murphy had a fresh task for her.
“Your Prime Minister needs a projection, a future scenario, in 48 hours,” he told her.
McVernon’s colleague, mathematical biologist Professor James McCaw, was also on the road when he received the same news. The two long-time collaborators had little more than two days to get a brief to the federal government’s National Security Committee – a first stab at how the alarming new threat might evolve.
It was a curtain-raiser to what would prove to be the most destructive pandemic to sweep the world since the Spanish flu 100 years before.
McVernon, 50, and McCaw, 43, were as well-briefed as anyone in the country on the rapidly emerging but as-yet-unnamed novel coronavirus. Both were members of an international network of modellers convened by the World Health Organisation (WHO) and had been dialling into the network’s meetings (usually held late at night, Australian time) since January 17.
“The modelling community had clocked very quickly that this was going to be bad and it was going to be long,” recalls McVernon, who is director of epidemiology at Melbourne’s Doherty Institute.
“It was clear we had to adopt a high transmissibility scenario, higher than most of our flu scenarios. The key unknown was whether it could be transmitted before the onset of symptoms. If that was the case, it was going to be a lot harder to control.”
On January 21, Murphy had invoked the Biosecurity Act in preparation for possible border restrictions.
At 12.39am on February 1, McVernon fired off an email to Murphy, relaying the latest consensus from the modellers’ network that the new coronavirus had broken out beyond Wuhan, and had seeded throughout China. It had become blindingly clear that the virus was not just jumping from infected animal to human, but transmitting between people.
Murphy was getting similar intelligence from the federal health department’s crisis centre, known as the National Incident Room. He fed that to federal Health Minister Greg Hunt, who immediately briefed Prime Minister Scott Morrison. Canberra slammed on the brakes. By that afternoon, Australia’s borders to China had been closed.
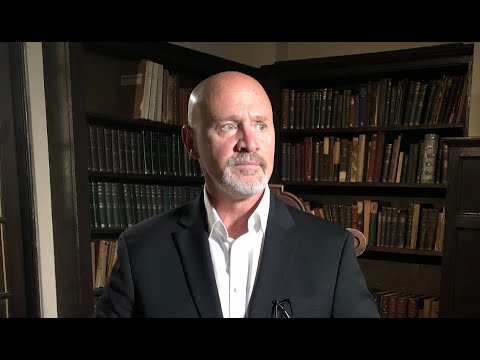
‘The modelling community had clocked very quickly that this was going to be bad and it was going to be long.’
Professor Jodie McVernon
But the virus had already slipped into the country, hitchhiking in the body of a passenger from Wuhan who had flown to Melbourne on January 19. Australia had its patient zero.
On February 11, the WHO christened the baffling new affliction “COVID-19”, a name that would dominate humanity’s waking hours and darken its collective dreams for the rest of 2020. The virus that caused it became labelled SARS-CoV 2. The silent invader would soon breach the defences of every country, though some – too tardy, in denial, under-resourced or poorly prepared – would fare much worse than others.
McVernon and McCaw had been invited onto the Australian Health Protection Principal Committee, the body which brings together federal, state and territory chief health and medical officers. It would meet seven days a week for more than four months, the pressure cooker atmosphere akin to a war cabinet. “Every day there was something new, the situation was changing so quickly,” says McCaw.
By the end of March, Australia had notched up 4500 cases – most, like the Wuhan traveller, introduced from overseas. Italy and Spain were becoming horrifying demonstrations of what could happen when rampant infection took hold. Exhausted physicians in those countries were running out of ventilators and intensive care beds, having to play God, and decide which of their patients lived or died.
With Australia’s case numbers doubling every three to five days in mid-March, some feared similar scenarios could unfold here. The federal deputy chief medical officer, Professor Paul Kelly, appeared to endorse speculation that between 20 and 60 per cent of the population might end up contracting the virus should it run wild. That generated headlines that fatalities could run as high 150,000 people.
The ABC’s coronavirus guru, Dr Norman Swan, warned publicly that NSW could be out of ICU beds within weeks if the sharp rise in cases continued. The federal Department of Home Affairs, which had the lead in managing emergency logistics, began searching for cold storage facilities where bodies could be stored if mortuaries were over-run.
McCaw insists now that those worst-case scenarios were never going to play out here. “Those figures showed what could happen if it was allowed to spread unchecked … [but] there was no way we were going to let it happen”.
NSW Chief Medical Officer Kerry Chant agrees: “It was never going to be acceptable to allow that spread, because that modelling was based on an unmitigated pandemic.” Instead, Australia’s political leaders bowed, almost always, to the medical advice.
The nation sealed off its external borders to all countries on March 20. Hotel quarantine was introduced. Social distancing and strictures on movement and economic activity were applied and then gradually eased as they started to “flatten the curve” of infection.
Then came Victoria’s outbreak, suppressed with one of the world’s harshest lockdowns. By November’s end, that state had managed the miracle of effective elimination of the virus from a community which, in August, had seen a peak of 725 new infections in a single day.
For McVernon, dealing daily with colleagues overseas where the virus is running rampant once again through the northern winter, it’s like inhabiting two separate universes.
“The idea that we would get to a [near] elimination state here didn’t seem plausible at the beginning,” she says. “It was very hard explaining to international colleagues just a month or so ago that we were in lockdown [in Melbourne] with five cases a day. What we take for granted now as our expected normal is so far apart from theirs.”
The Long COVID effect
Dr Sarah Coombes is a Sydney-based emergency services physician. Previously in robust health, the 54-year-old contracted COVID-19 in Europe in March, testing positive to the virus soon after arriving home.
Months later, she still suffers from COVID-related joint pain, managed with anti-inflammatories and Panadol, and increased heart rate and chest pain if fatigued. For six months she was at 75 per cent of her previous energy levels. Now it’s 90 per cent and some days worse than others.
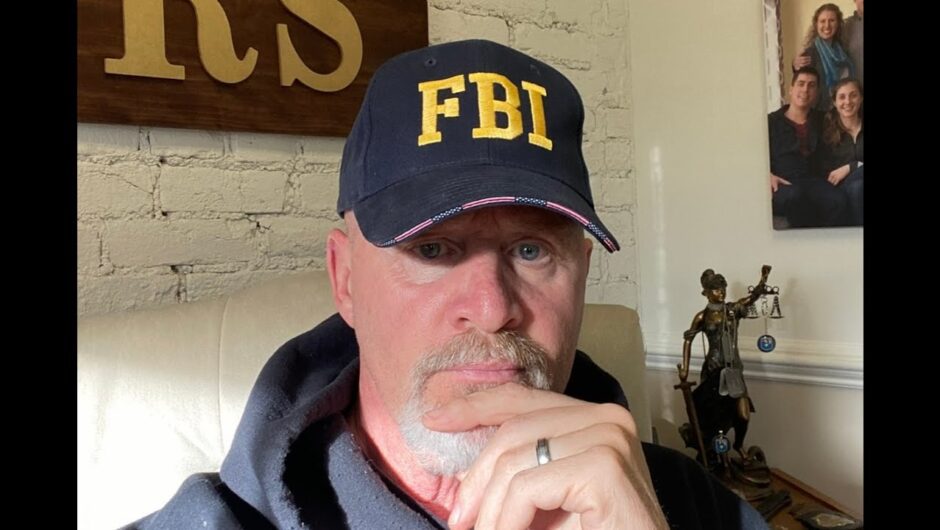
Emergency physician Dr Sarah Coombes has suffered the effects of Long COVID.Credit:Louise Kennerley
Coombes is a victim of what’s become known as “Long COVID”, a syndrome where patients remain afflicted with lingering effects long after they’ve ceased being infectious.
For some, it’s not just the physical toll, but the stigma as well. At St Vincent’s hospital in Sydney, where professors Gail Matthews and Greg Dore are running a study of some 140 Long COVID sufferers, some stories are heartbreaking: patients who’ve spent weeks isolated from family, friends and colleagues, longing for human touch from someone other than a figure clad head to toe in personal protective equipment.
There is the 60-year-old whose gardening business is floundering, because no one will hire him having heard he had contracted the disease. One couple’s children were made to sit metres away from classmates after their parents were diagnosed. Yet these people are probably among the safest company to be in if they have developed antibodies, says Dr Kari Lancaster, a UNSW social scientist who is attached to the St Vincent’s study.
Why an unlucky group suffers in this way (up to one in 20 will still have symptoms after eight weeks, according to one British study) is among the many mysteries still to be unlocked about the virus, even after a torrent of clinical trials, observational studies and autopsy examinations.
As well as being wildly infectious, the virus is fickle. It strikes a minority (mostly in older age groups) with lethal effect, while about 80 per cent will have mild symptoms or none at all.
That’s an “incredibly disruptive” combination of characteristics, says McCaw: “There are enough cases of low-level symptom or asymptomatic transmission that it spreads easily, yet is very, very severe for the vulnerable”.
Thought at first to spread mainly by way of surface and physical contact early in the pandemic, the evidence has become overwhelming that it’s remarkably efficient at transmitting through aerosols – the tiny droplets we exhale, particularly when exercising, singing, and talking loudly in indoor environments. (Belatedly, WHO recommended mask wearing in public in early June.)
Loading
The disease at first seemed to affect just the lungs. “But we quickly learned it affects every single organ system,” says Dr Neha Dangayach, co-director of neurosurgical intensive care at Mount Sinai Hospital in New York. There were gastro and cardiac and neurological presentations. Doctors across the globe were reporting the same myriad complaints.
WHO’s list of COVID symptoms grew from a handful of respiratory complaints to include headache, muscle and joint pains, nausea, diarrhoea, vomiting, loss of sense of smell and/or taste, loss of appetite and fatigue, conjunctivitis, discolouration of fingers and toes, chest pain or pressure and loss of speech or movement.
Australian neuroscientist Thomas Oxley, in the neurosurgery department at Mount Sinai, documented a spike in strokes among younger COVID-19 patients who had been asymptomatic or presented with mildest of symptoms.
Chant says: “I don’t think there’s ever been an experience where it has been such a prolonged period of continual learning.”
While many treatments have been tried, no cure has emerged. A handful of therapeutic approaches appear to help stave off severe disease, if administered early enough.
But outgoing US president Donald Trump’s favourite, hydroxychloroquine, proved to be a dud. Today, almost all trials of hydroxychloroquine have been halted, amid a volley of accusations between scientists of poorly designed trials and vested interests.
As Professor of Surgery at Sydney University Henry Woo told The Sydney Morning Herald and The Age in April, “there are a lot of things that can destroy the virus in a Petri dish – like kerosene”. Trump’s doctors seem to have had more success with a monoclonal (lab-engineered) antibody called REGN-COV-2, though it’s still experimental.
Professor Steven Tong, who is leading a clinical trial dubbed ASCOT at the Doherty Institute, says two drugs have emerged as solid treatment options: dexamethasone and the antiviral Remdesivir. Both are routinely given to hospitalised COVID patients in Australia and internationally.
Remdesivir appears to shorten the duration of the hospital stay of COVID-19 patients, according to one US study. But the WHO’s SOLIDARITY trial delivered a less glowing assessment, finding it did not reduce mortality.
“It doesn’t stop people from dying, but for hospitalised patients needing oxygen therapy, but not sick enough to need ventilation it appears to speed up their time to discharge compared to patients given placebo,” Tong says.
Dexamethasone, on the other hand, does appear to save lives, according to investigators of the RECOVERY trial, a cornerstone of COVID-19 treatment research, which has recruited more than 14,000 patients from across the UK’s National Health Service. It reduces deaths by one-third among ventilated patients and one-fifth in patients receiving oxygen therapy. The Australian ASCOT trial is currently testing convalescent plasma – blood plasma rich in antibodies collected from donors who have recovered from COVID-19.
With therapeutics still so far from delivering the magic solution, all eyes are now on vaccines, with three of the frontrunners delivering huge promise in recent weeks.

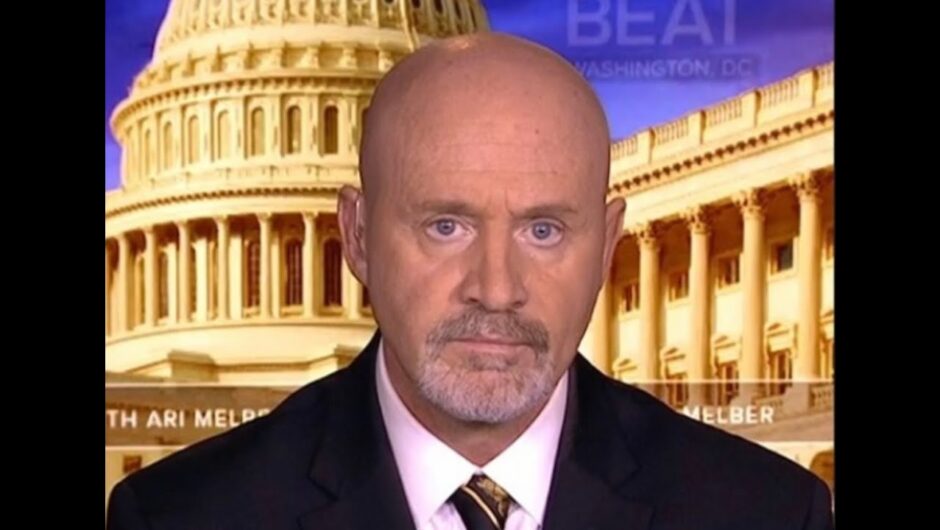
Staff at CSL in Melbourne prepare to manufacture the AstraZeneca-Oxford University COVID-19 vaccine.Credit:Getty Images
Two of these – one produced by Moderna, and the other by Pfizer, both based in the US – represent a breakthrough in modern vaccine technology, using messenger RNA (mRNA) to instruct human cells to manufacture parts of the virus in order to rouse the body’s own immune response.
Both look to have a 94-95 per cent effectiveness rate. The third, made by AstraZeneca in conjunction with Oxford University, reported about 70 per cent effectiveness (though it is currently subject to further testing), and would be cheaper and easier to distribute.
But the big “if” is whether these or other vaccines still in the pipeline will prevent infection, as well as the disease caused by the virus.
Canberra is hedging its bets and has invested more than $3.2 billion on four vaccine candidates thus far, including the Pfizer and AstraZeneca products. However as US infectious diseases authority Dr Anthony Fauci has warned, “the cavalry is coming, but don’t put your weapons down”.
While they may protect against the disease caused by the virus, it’s not clear for how long. Nor is it yet clear whether they can stop transmission – the only thing that can bring the virus to a shuddering halt.
Even after prolonged safety trials, the risk of extremely rare side effects may not be known for some time. Then there’s vaccine hesitancy, which seems to be growing in some sections of the population.
Professors Matthew Gray and Nick Biddle, social researchers at the Australian National University, found in their surveys that between 12 and 13 per cent of adult Australians would definitely or probably not get vaccinated against COVID-19.
Our Achilles’ heel
Quarantine hotels remain our Achilles’ heel, for as long as the virus runs rampant beyond our shores. Victoria graphically illustrated this, as did South Australia’s recent outbreak.
Chant worries about maintaining vigilance. “One of the things that we have been grappling with over recent weeks is how to keep [emphasising] the message that even one case matters,” she says.
Hunt wants to see Australia “at a place where we are as fully vaccinated as people choose … by the end of 2021”, starting as early as March. To this end, the safety watchdog, the TGA, has already granted AstraZeneca and Pfizer “provisional predetermination”, which could expedite approval.
But McVernon sounds a note of caution. “Realistically I think [the vaccines] will be one of a suite of ongoing risk reduction measures until we learn more about how effective they are. It’s likely that we will still need some degree of social constraint, and all those other COVID-safe practices … until we understand their impact on transmission. That will be the evolving story.”
Get our Coronavirus Update newsletter
Stay across the news you need to know related to the pandemic. Sent Monday and Thursday. Sign up here.
Deborah Snow is a senior writer for The Sydney Morning Herald.
Kate Aubusson is Health Editor of The Sydney Morning Herald.
Most Viewed in National
Loading