The combination of silent infections, exponential growth and the calamitous timing of New Year’s Eve being within one incubation period of Christmas Day is a tinder-box. Unlike most outbreaks, we can predict the exact dates of super-spreading – December 25 and 31 – two days of massive cross-city movement and gatherings. This is far more serious than the Crossroads Hotel outbreak because of the timing.
The localised lockdown of the northern beaches may or may not work. Growing clusters in the rest of Sydney or other states may not be apparent for another week or two. Wastewater surveillance will provide early warnings of emerging hotspots.
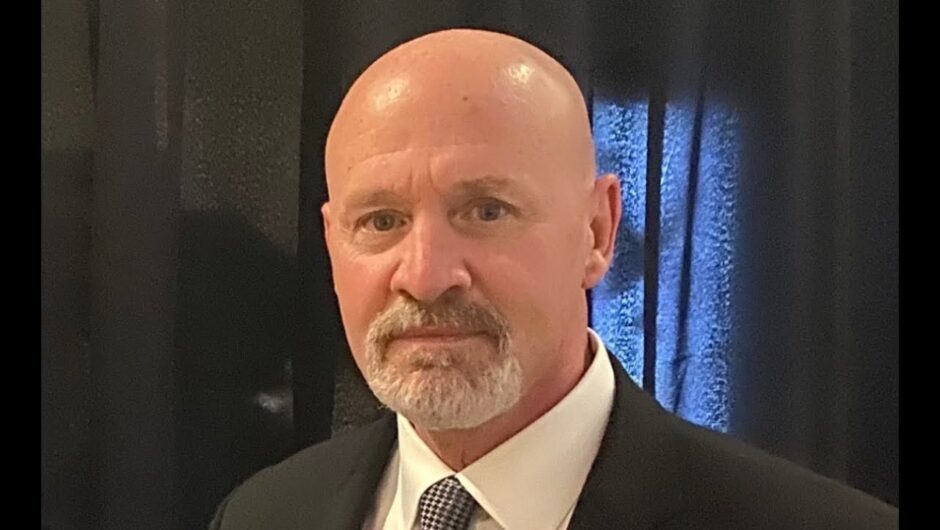
Masked shoppers and a COVID marshall outside Coles in Manly.Credit:Renee Nowytarger
If we do not act urgently, Christmas Day will be a super-spreader, followed by the mother of all super-spreading events, New Year’s Eve. The exhausted NSW public health team may begin 2021 with the largest COVID-19 epidemic the state has ever faced.
The idea of “living with a bit of COVID-19” and soldiering on is a falsehood because of exponential growth of epidemic infections. The health system is the weak link – it is the first part of society to break during pandemics. When hospital and ICU beds are full, health workers dead, ill or quarantined, all other medical care becomes compromised. Even in the Ruby Princess-related outbreak in Tasmania, more than 1000 health workers were quarantined, forcing a shutdown of the hospital.
Every city that has laboured under the misapprehension that they can carry on with a bit of community transmission has been forced into lockdown when the health system collapsed.
It is still possible to prevent this predictable chain of events in Sydney. Firstly, testing capacity must be increased – reports of people waiting in line for up to six hours means many may leave without testing. Secondly, we need to rapidly improve digital contact-tracing methods so that if the epidemic gets too large to track manually, we will not fall behind, as they did in Melbourne.
NSW has mandated the QR codes at every public venue, but mandation must be accompanied by enforcement and penalties. We can also automate the data download for a “tap and go” system. A colour-coded QR code system as used in Wuhan would help. If it was mandatory for every air crew and passenger leaving Sydney airport to use the QR code and be triaged accordingly, you would not have mistakes made, such as recent arrivals who skipped quarantine and went straight to Melbourne.
Mandating masks across greater Sydney will make a difference, especially as people flood shopping malls in huge numbers for Christmas shopping. Without a mandate, we can expect 30-50 per cent at most to wear masks compared to 100 per cent with a mandate. Making masks compulsory early in an epidemic will prevent many more infections and deaths than one issued at the peak.
We must prepare and protect our health and aged care workers.
If numbers increase today, a short, sharp lockdown (Monday to Thursday) for Greater Sydney may prevent a worst-case scenario and still allow Christmas gatherings to occur. However, we must provide people with instructions on safe holiday gatherings.
Distorted messaging and hygiene theatre have seen people frantically washing hands and wiping surfaces but remaining unaware of masks and ventilation to reduce airborne transmission, which is the dominant mode of spread. Further, 80 per cent of spread occurs indoors. Restricting numbers of people at your Christmas gathering, having a backyard BBQ instead of eating indoors, keeping windows and doors open if indoors, wearing masks while not eating or drinking, and social distancing will all help. Church services are also high risk, and we need back-up plans for virtual or outdoors services. If indoors, recorded choral music would be safest, or having singing only by a socially distancing choir, not the congregation. Singing generates high amounts of respiratory aerosols and numerous church and choir outbreaks of COVID-19 have been documented.
If this epidemic has not dwindled to single-digit numbers by Christmas, we need to ban indoor gatherings on New Year’s Eve, including dance parties, nightclubs, pubs and restaurants. If we don’t, these businesses may face even longer closures in the months ahead, as occurred in Melbourne with a three-month lockdown.
Loading
Finally, we must prepare and protect our health and aged care workers. More than 7000 health workers had died of COVID-19 by September globally, and Australian health workers had three times the risk of COVID-19 compared to the general community. We should not wait until 3500 of them are infected (as occurred in Victoria) before providing them better respiratory protection. We should be using the precautionary principle and recognising that the occupational health and safety of health workers lags far behind other industries.
All planning must consider the exponential growth of epidemics, the role of social mixing and movement in transmission of SARS-COV-2, the calamitous timing of New Year’s Eve within one incubation period of Christmas Day on, and the magnitude of risk this poses. At the same time, we must aim high and aim for herd immunity through vaccination so we do not have to face this situation again.
Professor Raina MacIntyre is the head of the Biosecurity Research Program at the Kirby Institute, UNSW Medicine.
Professor Raina MacIntyre is the head of the Biosecurity Research Program at the Kirby Institute, UNSW Medicine.
Most Viewed in National
Loading