coronavirus, covid, covid-19, coronavirus, canberra covid, covid expert, act health, karina kennedy, imogen mitchell
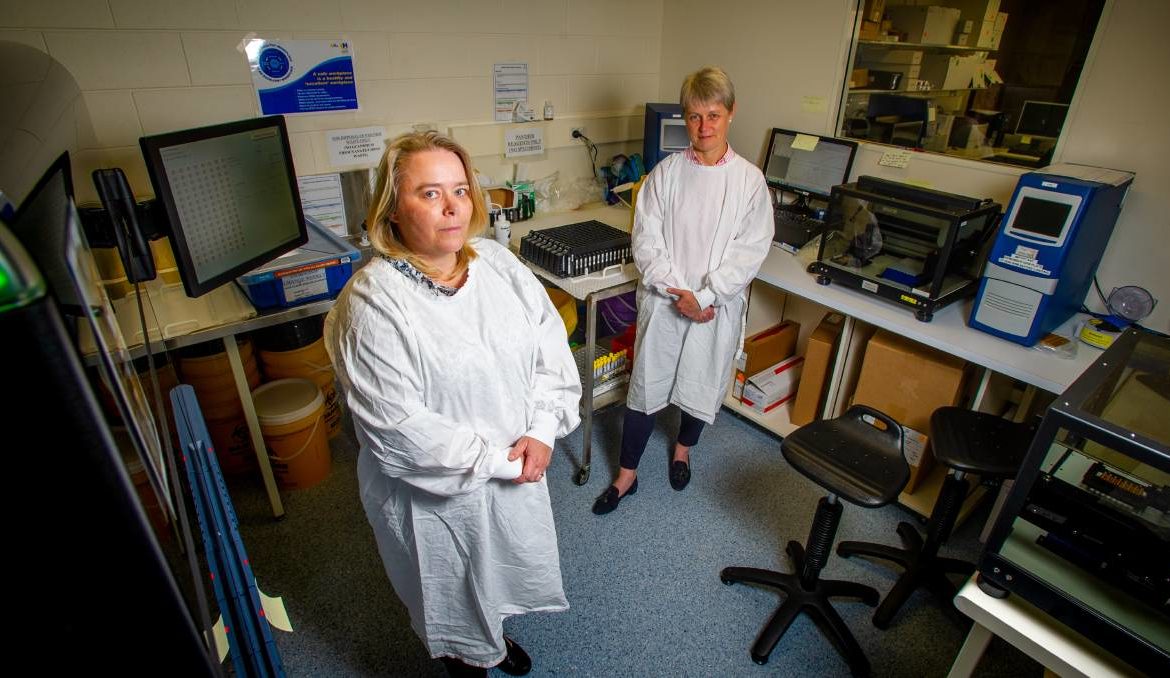
As a microbiologist and infectious disease expert, associate professor Karina Kennedy always anticipated the possibility of a pandemic outbreak. But she never foresaw just how large the COVID-19 pandemic would become. “I thought the scale of things would be big, but not this big and not for this long,” she said. “No one expected we would do the amount of testing we would be doing. Just when we thought we had reached our capacity, we had doubled that, and then we had doubled that again.” The associate professor has been one of the key people working behind the scenes as part of Canberra’s COVID-19 response, being the director of clinical microbiology at ACT Pathology. Ms Kennedy has been just one of the many people behind setting up diagnostic testing for coronavirus in the ACT, as well as helping to set up genomic testing for the virus. With the virus developing quickly across the community, she said a lot of the critical responses in the ACT had to be decided just as fast as the virus was able to spread in order to match it. “Everything was having to be done on the run, and provide diagnostics to people as they were still developing and testing [cases] while also looking at different technology,” she said. “It’s been this evolving thing over the past 10 months or so. “Ours was the first laboratory in Canberra to do COVID-19 testing and it’s been about ramping up our testing capacity.” While figuring out to do more tests more quickly was one of the challenges of the pandemic, with almost every country in the world ramping up their own COVID tests, determining how to gain access to testing supplies was also a critical challenge faced by those on the virus frontline. “In clinical areas you don’t often think about the supply aspect,” Ms Kennedy said. “We were getting low on testing reagents at some stage and they could run and these were produced globally and sent to Australia. “It was about diversifying testing techniques so you weren’t reliant on one single supply chain, so then some companies across Australia have started to produce things across Australia so we aren’t reliant on the rest of the world.” Professor Imogen Mitchell was also one of the many people on Canberra’s coronavirus front line, working as a clinical director to the ACT’s COVID-19 response. She said while the initial situation seemed daunting, response staff were keen to avoid situations of intensive care units at capacity like in Italy or the United States. “Originally, my role was providing the ACT with clinical advice for a response plan and we looked at how we could increase our own capacity for patients with COVID,” Prof Mitchell said. “Because we were all relatively new at managing a global pandemic, one of the things we learnt was that governance was important to helping manage who was doing what early on. “Dividing the health emergency response into two, a public and a clinical response, has been helpful.” Prof Mitchell said one of the biggest surprises during the pandemic was to see hope of wonder drugs to treat COVID-19 fall by the wayside and instead see a surge of reliance on public health measures. “A lot of people got excited at first at what different treatments there could be, and most of them were struck off as not being effective,” she said. “At the end of the day, what’s fascinating for me is watching how all the public health measures worked, and if people followed what public health experts told people to do, it helped to prevent COVID.” While there were many aspects of the pandemic that surprised critical health staff managing COVID-19, one thing that hasn’t has been Canberra, and indeed Australia’s, relative success in keeping the virus under control, as countries like the UK and US still battle rapidly rising infection numbers. “I think the Australian population really have to be congratulated in the way they have managed the pandemic,” Prof Mitchell said.
/images/transform/v1/crop/frm/Yb2Jn5LgcGxmVnDUUjd5xi/6322c70f-62b7-4fe1-a2c1-bbd74bd923de.jpg/r10_157_4146_2494_w1200_h678_fmax.jpg
As a microbiologist and infectious disease expert, associate professor Karina Kennedy always anticipated the possibility of a pandemic outbreak.
But she never foresaw just how large the COVID-19 pandemic would become.
“I thought the scale of things would be big, but not this big and not for this long,” she said.
“No one expected we would do the amount of testing we would be doing. Just when we thought we had reached our capacity, we had doubled that, and then we had doubled that again.”
The associate professor has been one of the key people working behind the scenes as part of Canberra’s COVID-19 response, being the director of clinical microbiology at ACT Pathology.
Ms Kennedy has been just one of the many people behind setting up diagnostic testing for coronavirus in the ACT, as well as helping to set up genomic testing for the virus.
With the virus developing quickly across the community, she said a lot of the critical responses in the ACT had to be decided just as fast as the virus was able to spread in order to match it.
“Everything was having to be done on the run, and provide diagnostics to people as they were still developing and testing [cases] while also looking at different technology,” she said.
“It’s been this evolving thing over the past 10 months or so.
“Ours was the first laboratory in Canberra to do COVID-19 testing and it’s been about ramping up our testing capacity.”
While figuring out to do more tests more quickly was one of the challenges of the pandemic, with almost every country in the world ramping up their own COVID tests, determining how to gain access to testing supplies was also a critical challenge faced by those on the virus frontline.
“In clinical areas you don’t often think about the supply aspect,” Ms Kennedy said.
“We were getting low on testing reagents at some stage and they could run and these were produced globally and sent to Australia.
“It was about diversifying testing techniques so you weren’t reliant on one single supply chain, so then some companies across Australia have started to produce things across Australia so we aren’t reliant on the rest of the world.”
Professor Imogen Mitchell was also one of the many people on Canberra’s coronavirus front line, working as a clinical director to the ACT’s COVID-19 response.
She said while the initial situation seemed daunting, response staff were keen to avoid situations of intensive care units at capacity like in Italy or the United States.
“Originally, my role was providing the ACT with clinical advice for a response plan and we looked at how we could increase our own capacity for patients with COVID,” Prof Mitchell said.
“Because we were all relatively new at managing a global pandemic, one of the things we learnt was that governance was important to helping manage who was doing what early on.
“Dividing the health emergency response into two, a public and a clinical response, has been helpful.”
Prof Mitchell said one of the biggest surprises during the pandemic was to see hope of wonder drugs to treat COVID-19 fall by the wayside and instead see a surge of reliance on public health measures.
“A lot of people got excited at first at what different treatments there could be, and most of them were struck off as not being effective,” she said.
“At the end of the day, what’s fascinating for me is watching how all the public health measures worked, and if people followed what public health experts told people to do, it helped to prevent COVID.”
While there were many aspects of the pandemic that surprised critical health staff managing COVID-19, one thing that hasn’t has been Canberra, and indeed Australia’s, relative success in keeping the virus under control, as countries like the UK and US still battle rapidly rising infection numbers.
“I think the Australian population really have to be congratulated in the way they have managed the pandemic,” Prof Mitchell said.