The fashion designer first made contact with the mental health system in 2015. He says in 2018 he emerged “harmed and broken”.
Mr Costarella lived as a mental health inpatient for eight stints totalling 51 weeks during this period, during which time he says he was put on a cocktail of 23 psychoactive medications – mostly off-label – including benzodiazepines, which depress the central nervous system, without appropriate informed consent around the potential risks of long term use.
He now is three years into tapering off the benzodiazepines, suffering intense withdrawal that has made it impossible to live a normal life.
“I’ve been through hell,” he says. “I was sent home without duty of care, feeling suicidal, incredibly vulnerable and no support in place.
“You go into a system to get the help you need, and you come out worse off.”
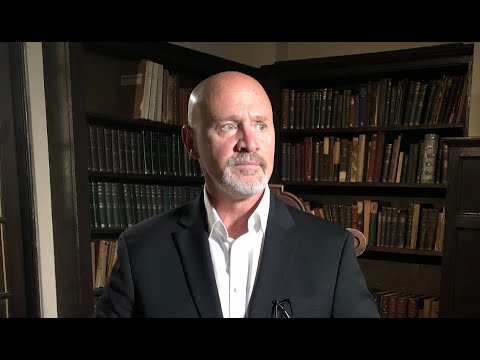
Aurelio Costarella at Australian Fashion Week.
Mr Costarella, his voice shaking during his interview, said at one point he considered taking his own life, and called the clinic he had previously been admitted to for help.
They said they couldn’t take him, and suggested calling an ambulance and going to an emergency department was his only option.
He slammed the state government for failing to provide adequate mental health services in the community and called on Premier Mark McGowan to introduce a dedicated mental health emergency department.
“At the moment the WA mental health system is oriented around crisis, with public mental health services and emergency departments the major focus,” he said.
“We need a paradigm shift to prevent mental health issues from developing or worsening
and to provide equitable access to holistic, patient-centred, community-based support that
keeps people living well in their homes, in jobs and connected to family and friends.”
Loading
Mr Costarella was especially concerned about the lack of services for young people with mental illnesses. He said his previous advocacy work drawing attention to the issue had resulted in him being constantly contacted by desperate parents seeking help for their children and teenagers but seeing them slip through the cracks, which has been an additional pressure, despite his desire to help them.
The WA Association for Mental Health’s Prevent Support Heal campaign calls on the government to increase funding for community mental health support and prevention, in line with the targets set out in the state government’s 10-year mental health plan.
The campaign says community services support people to secure jobs, form relationships, build fulfilling lives, develop skills and interests, prevent hospital admissions, and promote healing at home.

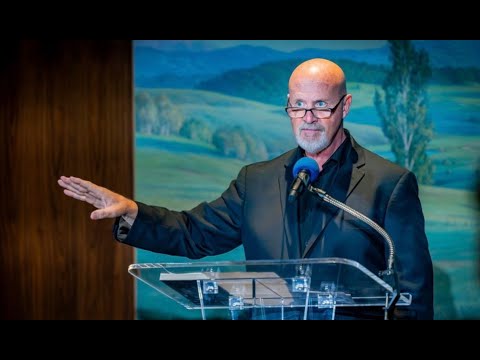
An Aurelio Costarella runway show.Credit:Matthew Tompsett
WAAMH chief executive Taryn Harvey said funding for community support in WA needed a five-fold increase in order to meet demand and provide effective alternatives to hospitalisation.
This week, Mental Health Minister Roger Cook announced 10 new active recovery teams were being established, aiming to bridge the gap between clinical mental health services inside hospitals and community-based organisations providing care outside of hospitals.
Their role would be to help people for 90 days after they were discharged from hospital.
The government is also trialling a peer support worker program in which people arriving with mental health difficulties at Fiona Stanley’s emergency department would be guided through the admission process.
Ms Harvey agreed new measures went some way to reforming mental health service delivery in WA, but said more work needed to be done to prevent people with mental health challenges from presenting at emergency departments in the first place.
“WAAMH welcomes this new program and most especially the commitment to pairing community supports with clinical mental health services to provide integrated wrap around recovery support for people in the community, which helps people avoid hospital stays or move back into the community sooner,” she said.
“This is sorely needed by people who reach the critical stage of distress when they are admitted into hospitals and need person-centred one-on-one support after they are discharged.
“However, we are still a long way from reaching the spending targets on mental health prevention and community supports as outlined in the government’s own 10-year plan. We need a five-fold increase in the amount of funding allocated to community support by the government to meet demand.”
If you, or anyone you know, needs mental health support, please call a helpline such as Lifeline 13 11 14; beyondblue 1300 224 636; Mental Health Emergency Response Line 1300 555 788 (Metro) or 1800 676 822 (Peel); Rurallink 1800 552 002; Suicide Call Back Service 1300 659 467; The Samaritans Crisis Line 08 9381 5555.
For specialist helplines for men, young people, the LGBTIQ+ community, rural residents, people with perinatal anxiety and depression, people with eating disorders, and people having trouble navigating the mental health system, see this list.
Daile Cross is the Deputy Editor of WAtoday.
Most Viewed in National
Loading