First, a growing number of countries around the world have decided against authorising the vaccine for people aged over 65 – the very group most at risk of serious illness and death from COVID-19.
Second, the rise of variants appears to cut the efficacy of the vaccine. We still don’t know by how much – but we now have several points of human data, none of them positive. South Africa, where one variant runs rampant, has paused the rollout of the vaccine.
On February 4 the federal government announced it had managed to score another 10 million doses of Pfizer’s vaccine. The government says it expects AstraZeneca to be approved for all age groups. But the timing, nevertheless, seems curious.
Problem 1: will the vaccine be approved for over-65s?
About 1.4 per cent of people aged over 65 who catch COVID-19 will die from it; that number rises to 15 per cent for people aged 85. So vaccinating older people is very, very important.
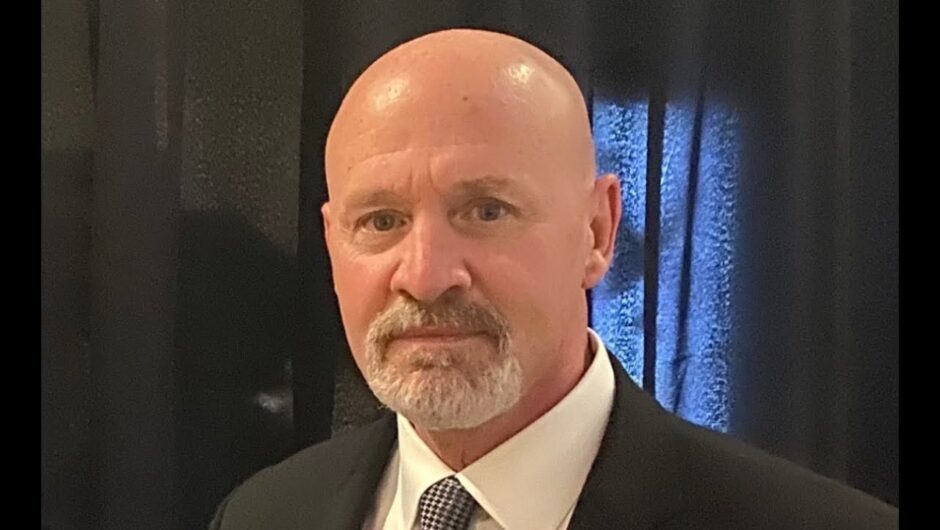
A nurse prepares a dose of the AstraZeneca COVID-19 vaccine in Oxford, England, last month.Credit:AP
So why have medical regulators from France, Germany, Austria, Sweden, Norway, Denmark, Netherlands, Spain and Poland decided against giving the AstraZeneca vaccine to the over-65s, as the BBC has reported?
The answer is found in table one of AstraZeneca’s phase three clinical trial report, published in the Lancet.
The trial enrolled 11,636 people in Britain and Brazil. But just 767 people from that group were aged between 56 and 69. Just 444 were aged over 70. And remember, this group includes people given a placebo, too.
It’s just not that much data. To make calculations of efficacy, vaccine trials look at the number of people who fell sick, rather than the number of people in the overall trial. AstraZeneca’s trial recorded just five cases in people aged over 55, and just two cases in people aged 65.
“The ability to draw conclusions is based not on the number of patients but on the number of people who have an event. It says there were five cases. It’s not going to be possible to draw any robust conclusions from that small number of cases,” says Vlado Perkovic, dean of medicine at the University of NSW and one of Australia’s leading clinical trial experts.
Compare that with the Pfizer vaccine: 37,706 people enrolled in the trial, 15,921 of whom were aged over 55.

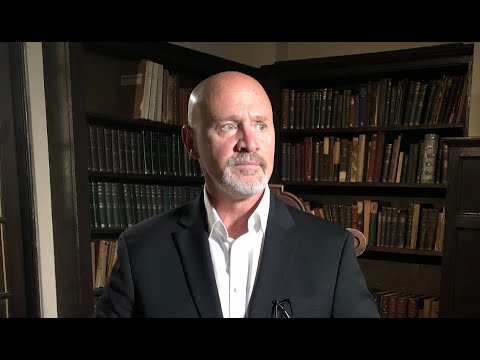
A medic administers a Moderna COVID-19 vaccine to a colleague in Bethlehem last week.Credit:AP
That does not mean the TGA is going to follow France and Germany’s lead. Britain, India, Mexico and Argentina, as well as the European Medicines Agency, have approved AstraZeneca’s vaccine for the over 65s. The question the TGA will ask, Professor Perkovic says, is not whether the vaccine works for people aged over 65, because we don’t know. It’s whether we have reason to believe it won’t work.
“When we look across all the vaccines, there is growing evidence they are effective in older populations. What we don’t know yet is whether one is more effective than the other. That’s interesting – but only if we have good reason to think one would be more effective than the other. And I’m not sure we do at the moment,” he says.
On a cellular level, we have good reason to think the AstraZeneca vaccine does work for older adults. Immune responses are the same across ages. Vaccines from Pfizer and Moderna and Russia’s Sputnik have reported no difference in efficacy among older groups.
Unless AstraZeneca can provide extra data – and it is working on it – to approve the vaccine for those aged 65-plus, the TGA will have to do some extrapolation.
“But this type of decision has to be made all the time. One example: Aboriginal Australians. They are unfortunately rarely represented in clinical trials in adequate numbers to know whether something works. We have to extrapolate,” says Professor Perkovic.
“This is such a compelling, traumatic problem, we’re going to have to make some judgment calls based on the best available evidence. I would personally support approval – it is a safe vaccine that is effective overall, and very likely to be equally effective in older people who are at highest risk from the disease. I don’t think it would be fair to make older people wait for more data before they can be vaccinated.”
Problem 2: those pesky variants
Scientists have been speculating for weeks about what effect the new variants of COVID-19 emerging around the world will have on vaccine efficacy.

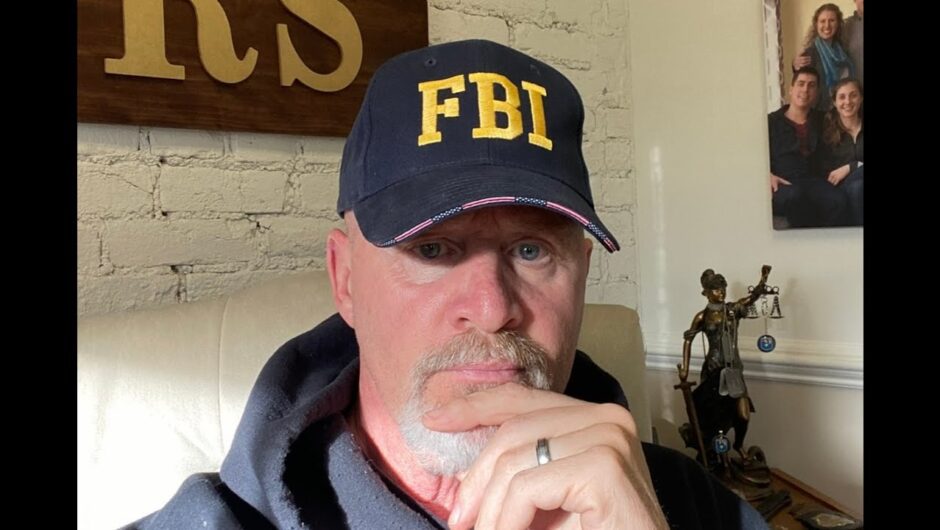
A South African woman walks past a coronavirus-themed mural promoting the use of face masks in public.Credit:AP
B.1.351, the variant first seen in South Africa, contains several mutations that look like they should limit antibody binding. The first tranche of data that emerged – lab tests of viruses made to look like the variants – seemed promising. The vaccines generate such strong immunity that even with a modest dip in efficacy they should still protect people.
Human data has not been so encouraging. Johnson & Johnson and Novavax both reported their vaccines were substantially less effective against the variant.
Now we have human evidence that the AstraZeneca vaccine may be hardest hit, after a South African trial put its efficacy against the variant at about 10 per cent.
Don’t put much weight in that exact number: the trial was so small the number is not statistically significant. But we now have three human studies showing a substantial drop-off in efficacy; AstraZeneca’s results are troubling enough for South Africa to pause the rollout of the vaccine.
AstraZeneca has already started work on a booster.
“These results are a reality check. It is time for us, unfortunately, to recalibrate our expectations of COVID-19 vaccines,” Shabir Madhi, who led the trial, said at a news conference organised by the South African National Department of Health.
Professor Madhi is right. These results should prompt us to think differently about our vaccines, in a couple of ways.
First, a lot of the focus has been on vaccines’ efficacy at preventing infection. But it’s becoming clear the first-generation vaccines are likely to struggle to do that, particularly as variants emerge (and more will emerge).
Loading
“Ultimately, the more important issue is: are we preventing serious illness? Because that is what is causing the biggest impact,” Trevor Drew, director of the CSIRO Australian Centre for Disease Preparedness, said this week.
So far, across all the trials, the vaccines seem to protect against severe illness and death, even if their efficacy differs.
Why? It might be that vaccine-induced T cells, rather than antibodies, are crucial for preventing severe disease and death. You’ll hear a lot more about that in coming weeks.
The second way we need to start thinking differently is to expect this virus to continue to circulate via antibody-resistant variants, with the potential that some people will have a vaccine that offers very little protection against infection.
The vaccines will not bring the pandemic to an end.
Examine newsletter
Science and health explained and analysed with a rigorous focus on the evidence. Examine is a weekly newsletter by science reporter Liam Mannix. Sign up to receive it every Tuesday.
Liam is The Age and Sydney Morning Herald’s science reporter
Most Viewed in National
Loading