Tens of millions of people around the globe have already received their COVID-19 vaccine and Australia’s is now set to begin.
But there is little testing data on those with certain medical conditions or within a particular section of the population – particularly pregnant women and the elderly.
Below, three health experts explain the official advice given by Australia’s federal health department and the Australian Technical Advisory Group on Immunisation (ATAGI).
I’m pregnant – should I get the vaccine?
ATAGI’s most updated advice for pregnant women getting the Pfizer/BioNTech vaccine is it does “not routinely recommend COVID-19 vaccine in pregnancy.”
This means that if you have no risk factors for severe COVID-19 or are not at high risk of exposure to the virus, you may prefer to wait until after your pregnancy.
Professor Julie Leask from the University of Sydney, who specialises in the uptake of vaccines, said it is not a cause for concern – the authorities are simply being “ultra-cautious”.
“The reason they’re not recommending it yet is because they haven’t actually done studies of the vaccine [on] its safety and effectiveness in pregnant women,” she said.
It’s true pregnant women have not been included in any of the major clinical trials of any of Australia’s vaccine candidates, so data on this group is scarce. But there have been several people who didn’t know they were pregnant or became pregnant during the trials in the US and UK, and scientists are monitoring them closely. So far, there have been no reports of adverse outcomes.
Professor Leask said she expects the advice for pregnant women to change over time when more data is assessed.
If you are at risk of severe disease from coronavirus, or you are at high risk of exposure to the virus, then vaccination is recommended, even if pregnant. The ATAGI said, “based on our understanding of this vaccine, we do not expect it to cause any serious problems in pregnant women or their babies.”
Will it affect my fertility or breastfeeding?
Professor Leask said recent data showing women in their 20s and 30s are some of the most likely to be feeling hesitant when it comes to the vaccine is unsurprising.
“There’s a little bit more hesitancy among females of childbearing age. We suspect that’s probably because they’re just wanting to be absolutely sure that the vaccine is going to be safe for them and their babies.”
According to the ATAGI’s advice, it absolutely is. It said the Pfizer/BioNTech vaccine will not affect a woman’s ability to become pregnant.
“There is no evidence that women who become pregnant after being vaccinated against COVID-19 have an increased risk of developing complications that affect their pregnancy or their baby’s health,” the advice states.
Similarly, breastfeeding mothers are also encouraged to get the vaccine. The advice suggests you do not need to stop breastfeeding before or after vaccination. Some were concerned the vaccine could pass through breastmilk, but ATAGI insists even if it did, it’s not a problem.
“The mRNA in Comirnaty [Pfizer/BioNTech] is rapidly broken down in the body and we do not think that it passes into breast milk. Even if it did, it would be quickly destroyed in the baby’s gut and is therefore extremely unlikely to have any effect on your baby,” ATAGI said.
I have bad allergies – should I get the vaccine?
The ATAGI’s advice suggests the Pfizer/BioNTech vaccine can be administered safely to people with allergies to food, insect stings and medicines.
The only people who might not be able to receive it are those who develop anaphylaxis after a previous dose, or have a history of anaphylaxis to any component of the vaccine, including polyethylene glycol (PEG).
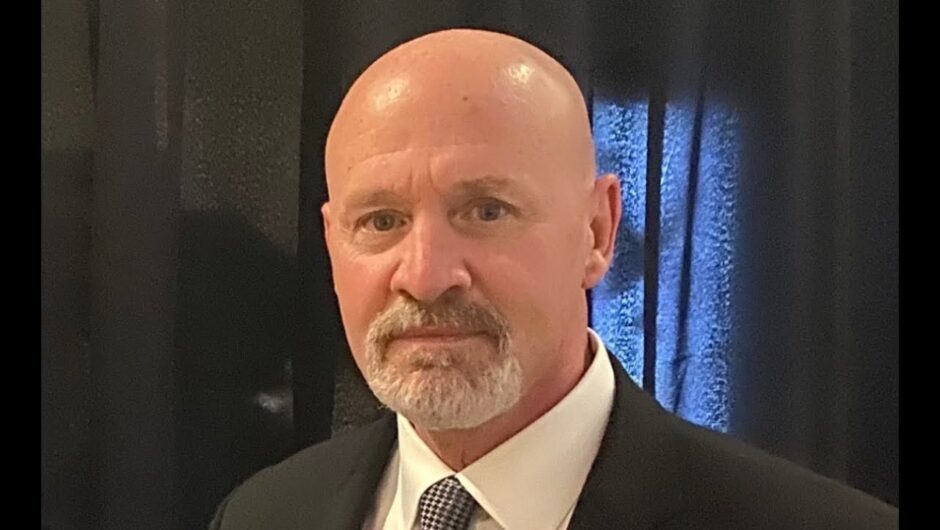
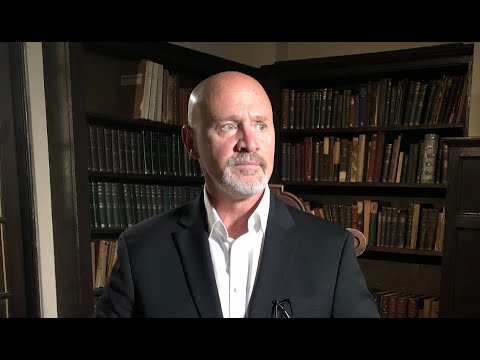
Professor Gary Grohmann, a virologist who has worked closely with the World Health Organisation and as a member for the Australian Immunisation Coalition, said allergic reactions are very rare.
“The rate is extremely low, which is fortunate; about 11 people per million,” he said.
“Nevertheless, it sends up a flag that anybody with allergy needs to talk to their doctor and those administering the vaccine need to be observing the vaccinee for 15 to 30 minutes.”
The ATAGI recommends anyone with a history of anaphylaxis, or those who have been prescribed an EpiPen, be observed for 30 minutes (rather than the usual 15 minutes) following their injection to be safe.
I’m immunocompromised, or have a medical condition, is it safe?
The Pfizer/BioNTech vaccine is recommended for people who are immunocompromised – especially given their increased risk of severe illness with the virus. The ATAGI did say though that there is currently no data on the safety and efficacy of the vaccine in this population because they were not included in clinical trials.
Professor Grohmann said anyone in this sector should speak to their doctor beforehand.
“While the data set is incomplete, it probably is still worth it from a risk assessment perspective to get the vaccine, but always go through your GP or health professional,” he said.
Professor Grohmann also noted the vaccine may be less effective and protective in this group because of a person’s reduced immune response.
“The efficacy for those that are immunocompromised will likely be lower, as well as the effectiveness,” he said.
“However, that doesn’t mean they’re not protected against major secondary endpoints to do with the severity of the disease like hospitalisation, ICU or even death.”
Is it safe for the frail and elderly?
The ATAGI has not released specific advice relating to frail elderly people, and instead advises each individual should be “carefully assessed on a case by case basis.”
Professor Grohmann said for this group, because of the impact of even relatively mild side effects, it’s important to balance the potential benefits with the potential risks.
“If somebody is particularly frail then maybe giving them a vaccine isn’t a good idea, so, therefore, ATAGI and others have advised it should be on a case by case basis,” he said.
Last month, reports that the Oxford-AstraZeneca vaccine, in particular, may not be safe for older people started circulating after multiple European countries only approved the vaccine for people under the age of 65.
But Professor Grohmann said: “we shouldn’t be alarmed by that, it’s simply a safety precaution because the data isn’t there”.
“We need more data to assess the effect of these vaccines in terms of efficacy and safety in the older person and in particular in those that are frail,” he said.
I’m scared of needles – what should I do?
Actually showing up and getting the injection can also be nerve-wracking for some people, especially if you’ve got a fear of needles.
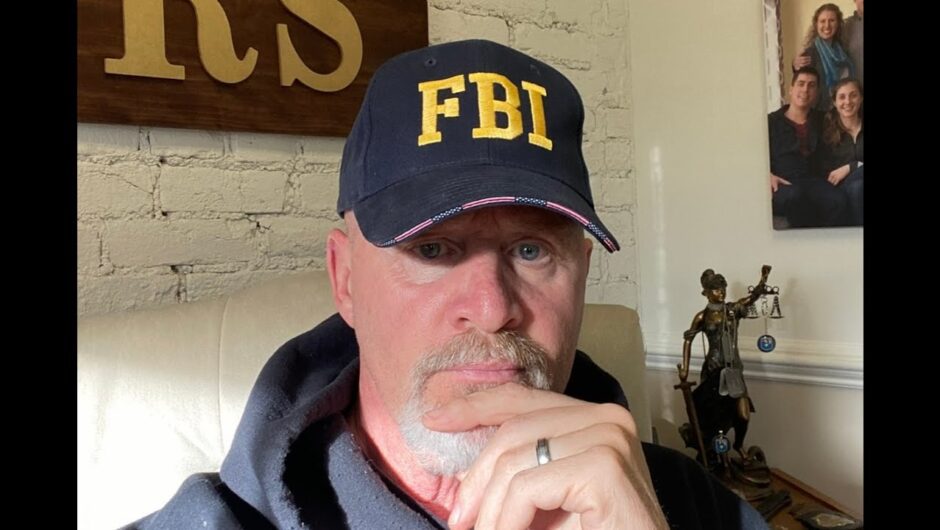
But Professor Adrian Esterman, an epidemiologist from the University of South Australia, said it’s nothing to worry about and “would be just like having a flu jab”.
Some people may experience mild side effects from the vaccine like soreness at the injection site or a headache, but they should all ease after a few days.
Professor Esterman said if you’re really concerned, speak to a professional.
“I know some people are very anxious about getting any sort of jabs, so probably speak to your doctor or psychologist to try and allay those fears,” he said.
I worry I’ll get exposed to the virus – is this possible?
Professor Esterman said catching the virus from any of the vaccines is impossible.
“None of the vaccines are live viruses, so there’s simply no chance that they would actually catch the infection through having the vaccine.”
And as for potentially picking up COVID-19 whilst at a vaccination centre, people shouldn’t be too concerned. Public health measures including mask-wearing and social distancing will no doubt be strictly enforced.
“In terms of vaccination centres, I assume people would be asked to wear masks where necessary and take the usual precautions,” Professor Esterman said.
What about my data – will it be stored by the government?
The government will store some information on you when you get vaccinated in order to keep track of who has had it.
“There is a national registry for vaccination, which will contain what vaccinations you’ve had, the date of them, presumably your date of birth and potentially any allergic reactions you might have had in the past,” Professor Esterman said.
It’s important for the government to have some data on your vaccination so they can follow up with any symptoms you might have down the track.
Can I get the flu jab as well?
The ATAGI recommends people should wait 14 days between both the Pfizer/BioNTech and the AstraZeneca jab, and receiving the flu jab. It said co-administration of two vaccines can “sometimes lead to a higher frequency of mild to moderate adverse events”, so it’s safer to wait.
Professor Grohmann agreed. “A two-week gap is cautionary and I think that’s sensible,” he said.
While the ATAGI “doesn’t recommend” getting both the COVID-19 and flu vaccines on the same day, it said there could be circumstances where co-administration of the vaccines could be considered.
Can I still donate blood?
The Australian Red Cross Lifeblood is asking donors to wait seven days from the time they receive their vaccine before they donate. After that, it’s fine.
Professor Grohmann said this is most likely to make sure the person isn’t experiencing any side effects.
“If the person receiving the vaccine is going to have any sort of reaction or illness or side effect, that’s going to come up within the first few days to a week,” he said.
“I think for that reason, there should be a space between getting the vaccine and donating blood.”
You may have noticed SBS News is no longer available on Facebook.
Here’s where else you can find our content and follow us:
People in Australia must stay at least 1.5 metres away from others. Check your jurisdiction’s restrictions on gathering limits.
If you are experiencing cold or flu symptoms, stay home and arrange a test by calling your doctor or contact the Coronavirus Health Information Hotline on 1800 020 080.
News and information is available in 63 languages at sbs.com.au/coronavirus
Please check the relevant guidelines for your state or territory: NSW, Victoria, Queensland, Western Australia, South Australia, Northern Territory, ACT, Tasmania