news, latest-news, borderline personality disorder, bpd, mental health canberra, mental health act
There are a host of “lost souls” in Canberra who could be helped out of their torment if specialist medical care was available, according to one of those people who is finding her way back to mental health and strength. Morgan Bayer suffers from borderline personality disorder, an illness marked by changing moods and cycles of anger and depression. Sufferers sometimes have suicidal thoughts. From her teenage years on, she would end up in hospital after self-harming. She uses the phrase “lost soul” about people who suffered like she did. She dropped out of high school in year 8. She was trouble and her mind was troubled. But she wasn’t just a difficult teenager. She was finally diagnosed with BPD which is defined as “a serious mental illness that centres on the inability to manage emotions effectively”. Once she was diagnosed, it became easier to address the issues. She sought the support of others in a similar plight and learned how to manage the condition. Morgan is now coming out of it, despite more than her fair share of hardship. She worked for eight years serving in a cafe until COVID-19 took the job away. But her good fortune was to meet Natalie Malcolmson whose husband, Todd, suffered from the illness. It prompted Natalie to set up BPD Awareness ACT. At BPD Awareness ACT, there are sessions where sufferers meet. These sessions involve learning how to tolerate stress, regulate their own emotions and how to communicate easily and well with others. A central concept is “mindfulness” – staying in the present and not dwelling on the past or getting over-powered by worry about the future. They lean on each other. They learn how to deal with overpowering emotions. “It’s the most common mental illness. It’s the most dangerous and it’s the most recoverable,” Natalie Malcolmson said. “People with BPD live in hell and their families live in hell.” Her husband, Todd, didn’t get diagnosed until he was middle-aged. Until then, his heavy drinking and anger just seemed like bad behaviour. He ended up in the emergency room 14 times in eight months. But once he was diagnosed, the problems could be addressed and he could learn how to deal with them. “It was pretty much sheer hell. I did everything from alcohol abuse to self-harm but I didn’t know why,” Todd said. Natalie said: “The slightest scratch and everything overwhelms them. They fall apart. And it’s the most stigmatised of mental illnesses.” The stigma derives from difficult behaviour which others perceive as way out-of-line and which ought to be controllable (even though the person exhibiting the behaviour can’t control it). Common stereotypes include that BPD patients are dramatic, manipulative and attention-seeking. Natalie Malcolmson said the stigma extended even to the medical profession who misdiagnosed people with BPD. She said sufferers couldn’t understand or control emotions. The casualties were often the people who were closest to them. Through the sessions at BPD Awareness ACT and the friendships, Morgan Bayer has learned to cope with her BPD. She knows the dark moods will pass, for example. But she said if more formal support and understanding had been there earlier, she could have tackled her situation earlier and better. Psychiatrist Dr Philip Keightley, who lectures at the ANU Medical School, agreed. He said other cities in Australia like Adelaide and Sydney recognised BPD by providing publicly-funded specialist treatment. The ACT government doesn’t do that. He thinks it should. He was particularly concerned about mothers who suffered the anger and depression before and after childbirth and who then passed on trauma to the next generation. Their condition was often misdiagnosed so they were given medication when they may need advice and counselling. There is private treatment available in Canberra for sufferers of BPD but Natalie Malcolmson said it was beyond the financial reach of many of the very people who needed it most, those mothers struggling to keep their heads above water and unable to cope with the mental pressure.
/images/transform/v1/crop/frm/fdcx/doc7ddn7gkzumr1gse06cct.jpg/r0_152_3000_1847_w1200_h678_fmax.jpg
There are a host of “lost souls” in Canberra who could be helped out of their torment if specialist medical care was available, according to one of those people who is finding her way back to mental health and strength.
Morgan Bayer suffers from borderline personality disorder, an illness marked by changing moods and cycles of anger and depression. Sufferers sometimes have suicidal thoughts.
From her teenage years on, she would end up in hospital after self-harming. She uses the phrase “lost soul” about people who suffered like she did.
She dropped out of high school in year 8. She was trouble and her mind was troubled.
But she wasn’t just a difficult teenager. She was finally diagnosed with BPD which is defined as “a serious mental illness that centres on the inability to manage emotions effectively”.
Once she was diagnosed, it became easier to address the issues. She sought the support of others in a similar plight and learned how to manage the condition.
Morgan is now coming out of it, despite more than her fair share of hardship. She worked for eight years serving in a cafe until COVID-19 took the job away.
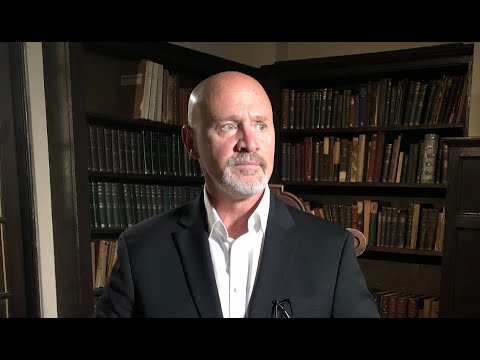
Morgan Bayer says that stress exacerbates her borderline personality disorder. Picture: Sitthixay Ditthavong
But her good fortune was to meet Natalie Malcolmson whose husband, Todd, suffered from the illness. It prompted Natalie to set up BPD Awareness ACT.
At BPD Awareness ACT, there are sessions where sufferers meet. These sessions involve learning how to tolerate stress, regulate their own emotions and how to communicate easily and well with others.
A central concept is “mindfulness” – staying in the present and not dwelling on the past or getting over-powered by worry about the future.
They lean on each other. They learn how to deal with overpowering emotions.
“It’s the most common mental illness. It’s the most dangerous and it’s the most recoverable,” Natalie Malcolmson said.
“People with BPD live in hell and their families live in hell.”
Her husband, Todd, didn’t get diagnosed until he was middle-aged. Until then, his heavy drinking and anger just seemed like bad behaviour. He ended up in the emergency room 14 times in eight months.
But once he was diagnosed, the problems could be addressed and he could learn how to deal with them.
“It was pretty much sheer hell. I did everything from alcohol abuse to self-harm but I didn’t know why,” Todd said.
Natalie said: “The slightest scratch and everything overwhelms them. They fall apart. And it’s the most stigmatised of mental illnesses.”
The stigma derives from difficult behaviour which others perceive as way out-of-line and which ought to be controllable (even though the person exhibiting the behaviour can’t control it).
Common stereotypes include that BPD patients are dramatic, manipulative and attention-seeking.
Natalie Malcolmson said the stigma extended even to the medical profession who misdiagnosed people with BPD.
She said sufferers couldn’t understand or control emotions. The casualties were often the people who were closest to them.
Through the sessions at BPD Awareness ACT and the friendships, Morgan Bayer has learned to cope with her BPD. She knows the dark moods will pass, for example.
But she said if more formal support and understanding had been there earlier, she could have tackled her situation earlier and better.
Psychiatrist Dr Philip Keightley, who lectures at the ANU Medical School, agreed. He said other cities in Australia like Adelaide and Sydney recognised BPD by providing publicly-funded specialist treatment. The ACT government doesn’t do that. He thinks it should.
He was particularly concerned about mothers who suffered the anger and depression before and after childbirth and who then passed on trauma to the next generation. Their condition was often misdiagnosed so they were given medication when they may need advice and counselling.
There is private treatment available in Canberra for sufferers of BPD but Natalie Malcolmson said it was beyond the financial reach of many of the very people who needed it most, those mothers struggling to keep their heads above water and unable to cope with the mental pressure.
- Support is available for those who may be distressed by phoning Lifeline 13 11 14; Mensline 1300 789 978; Kids Helpline 1800 551 800; beyondblue 1300 224 636; 1800-RESPECT 1800 737 732.