news, health, palliative care, Calvary, TCH, Canberra Hospital
Palliative care doctors and nurses are being stretched too thin to cope with their workloads, as the country struggles through a severe shortage of specialised staff. Research published by the Australian Catholic University this week shows there is currently less than one full-time palliative care physician for every 100,000 people in Australia. That number needs to be more than doubled for it to meet industry benchmarks, as demand for palliative care has increased dramatically. Australian Medical Association ACT president Dr Antonio Di Dio suggested the issue had extended to Canberra. “I’ve not seen enough evidence of an on-the-ground increase in staff numbers and hours in palliative care that is commensurate with growing demand,” he said. “In the last couple of years, the population of Gungahlin alone has increased by about 35,000 people. The population of Canberra is over 400,000. Only a decade ago, it was much, much different.” Dr Di Dio said palliative care staff, like those “amazing” ones at Calvary Hospital’s Clare Holland House, responded to shortfalls by “simply working harder”. He said the health sector needed to attract more palliative care physicians through advertising and promotion, but it was hard when workplaces were becoming less attractive. “The [present physicians] that we’ve got are brilliant and they need to be supported, but once you stretch them for too long, month after month, year after year, they get tired and work too hard,” Dr Di Dio said. “Other people who talk to them say, ‘Oh, the people in Canberra are overworked – I don’t want to work in Canberra because they’re overworked’, and so it becomes a sort of perpetuating spiral.” The university said the number of people being hospitalised for palliative care was growing at a rate of 5 per cent a year for adults, and 10 per cent a year for children. Report author Dr Cris Abbu said palliative care remained “one of the least preferred specialisations of medical students for future practice”, and the lack of community-based palliative care services in Australia meant there was a huge strain on the public health system. “We need to encourage more doctors and nurses to choose this important work,” Dr Abbu said. Calvary Public Hospital’s general manager Robin Haberecht was optimistic about the future of palliative care. She believed more people would pursue it as a career over time, particularly given talking about death and dying was becoming more common, and palliative care was getting more of a profile. “We are starting to see more innovation in the field,” Ms Haberecht said. “It is hard to be certain but in my experience there is a positive trend for health professionals wanting to work in palliative care as a specialty for nurses, doctors and allied health professionals.” She said palliative care and end-of-life patients did not place “a great deal of pressure” on Calvary’s inpatient capacity, and outreach and outpatient services were being provided to more than 750 people. “The acute care setting is rarely the best setting for palliative care patients once their symptoms are being managed or a health emergency is addressed,” Ms Haberecht said. She said Clare Holland House currently had 19 palliative care inpatient beds, and another eight were being added as part of its expansion project. The project is due to be completed by the middle of the year. Report authors at the university said Australia should introduce an active recruitment program with student scholarships and government subsidies to get another 225 specialist palliative care doctors working across the country. Our journalists work hard to provide local, up-to-date news to the community. This is how you can continue to access our trusted content:
/images/transform/v1/crop/frm/fdcx/doc76r42aziqt3hgwnhh5j.jpg/r0_47_3467_2006_w1200_h678_fmax.jpg
Palliative care doctors and nurses are being stretched too thin to cope with their workloads, as the country struggles through a severe shortage of specialised staff.
Research published by the Australian Catholic University this week shows there is currently less than one full-time palliative care physician for every 100,000 people in Australia.
That number needs to be more than doubled for it to meet industry benchmarks, as demand for palliative care has increased dramatically.
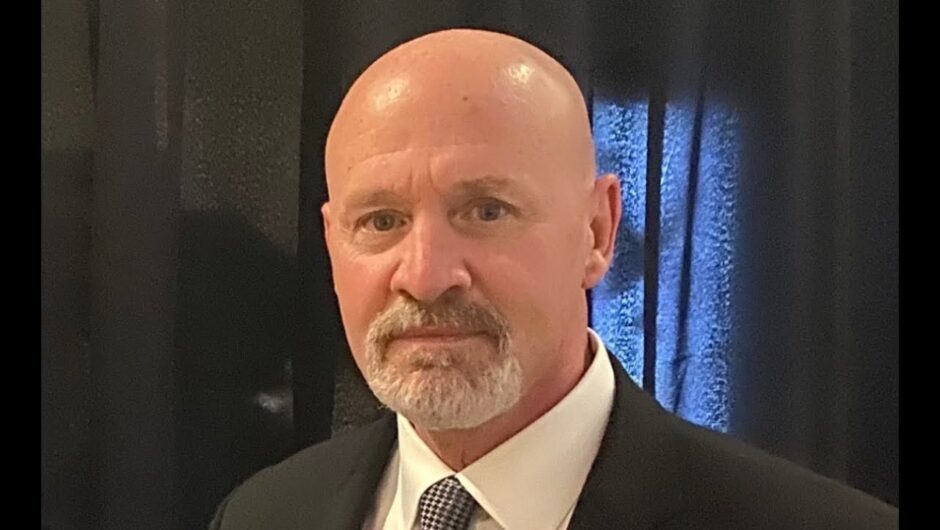
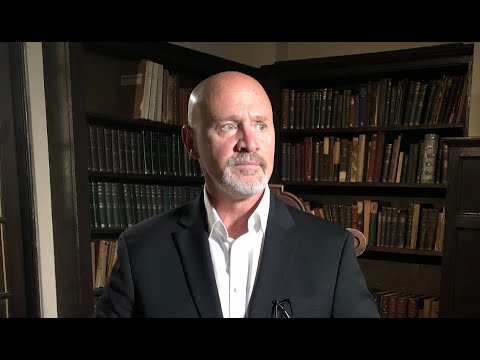
Australian Medical Association ACT president Dr Antonio Di Dio suggested the issue had extended to Canberra.
“I’ve not seen enough evidence of an on-the-ground increase in staff numbers and hours in palliative care that is commensurate with growing demand,” he said.
“In the last couple of years, the population of Gungahlin alone has increased by about 35,000 people. The population of Canberra is over 400,000. Only a decade ago, it was much, much different.”
Dr Di Dio said palliative care staff, like those “amazing” ones at Calvary Hospital’s Clare Holland House, responded to shortfalls by “simply working harder”.
He said the health sector needed to attract more palliative care physicians through advertising and promotion, but it was hard when workplaces were becoming less attractive.
“The [present physicians] that we’ve got are brilliant and they need to be supported, but once you stretch them for too long, month after month, year after year, they get tired and work too hard,” Dr Di Dio said.
“Other people who talk to them say, ‘Oh, the people in Canberra are overworked – I don’t want to work in Canberra because they’re overworked’, and so it becomes a sort of perpetuating spiral.”
The university said the number of people being hospitalised for palliative care was growing at a rate of 5 per cent a year for adults, and 10 per cent a year for children.
Report author Dr Cris Abbu said palliative care remained “one of the least preferred specialisations of medical students for future practice”, and the lack of community-based palliative care services in Australia meant there was a huge strain on the public health system.
“We need to encourage more doctors and nurses to choose this important work,” Dr Abbu said.
Calvary Public Hospital’s general manager Robin Haberecht was optimistic about the future of palliative care.
She believed more people would pursue it as a career over time, particularly given talking about death and dying was becoming more common, and palliative care was getting more of a profile.
“We are starting to see more innovation in the field,” Ms Haberecht said.
“It is hard to be certain but in my experience there is a positive trend for health professionals wanting to work in palliative care as a specialty for nurses, doctors and allied health professionals.”
She said palliative care and end-of-life patients did not place “a great deal of pressure” on Calvary’s inpatient capacity, and outreach and outpatient services were being provided to more than 750 people.
“The acute care setting is rarely the best setting for palliative care patients once their symptoms are being managed or a health emergency is addressed,” Ms Haberecht said.
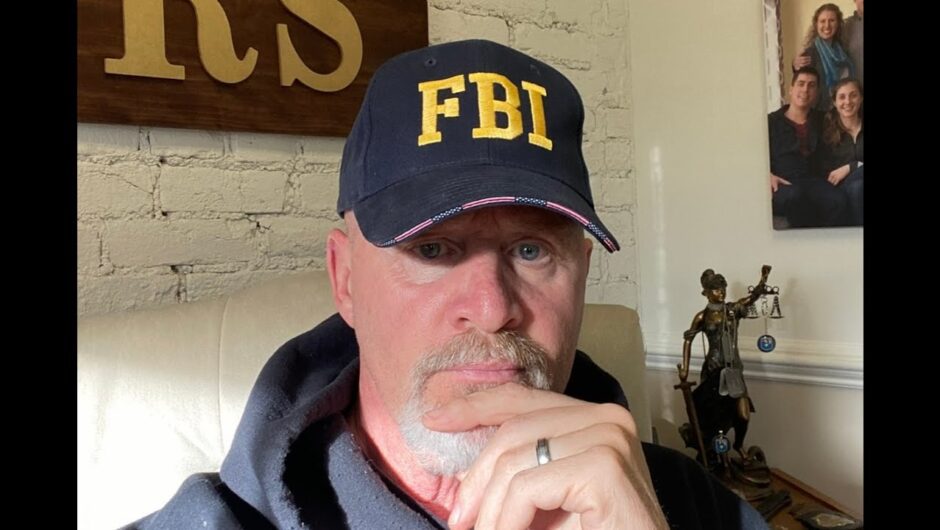
She said Clare Holland House currently had 19 palliative care inpatient beds, and another eight were being added as part of its expansion project.
The project is due to be completed by the middle of the year.
Report authors at the university said Australia should introduce an active recruitment program with student scholarships and government subsidies to get another 225 specialist palliative care doctors working across the country.
Our journalists work hard to provide local, up-to-date news to the community. This is how you can continue to access our trusted content:
ACT hospice Clare Holland House, which currently has 19 pallative care inpatient beds. Picture: Elesa Kurtz