coronavirus, how is covid tested, how do covid tests work, covid test canberra, how covid tests work canberra, how covid tests work
It’s the brief moment of discomfort more than 170,000 Canberrans have endured as part of the effort to keep a deadly pandemic in check. But what happens to the swab after it’s put so far enough up your nose your eyes begin to water? COVID-19 testing has been the key component of the large-scale public-health effort to reduce the coronavirus impact in Canberra. Canberra’s first COVID-19 test was conducted on February 10 last year. The first case was confirmed a month later on March 11. Since then, testing rates have ebbed and flowed – numbers rising to almost unmanageable peak levels after confirmed cases and then dropping to be almost non-existent when people become complacent. Professor Karina Kennedy, ACT Pathology’s director of clinical microbiology, has overseen a year of tremendous change, battling equipment shortages and demand spikes to keep test results flowing out smoothly. The lab was busy managing 250 tests a day 12 months ago. Now – thanks to additional staff – the lab can handle several thousand a day. “We only had seven existing staff in that area, so we were fortunate in that the hospital and Health supported us in being able to realise that we did more staff. So we were able to quickly train up a good group of people who could actually do that role,” Professor Kennedy said. “We wouldn’t have been able to do it with the existing staffing that we had, because it’s just such a small unit to start with.” In a year since the first tests were completed – at a time when scientists were still scrambling globally to understand much of the virus and the potentially fatal disease it causes – Canberra’s ability to process large batches of tests each day has surged ahead. It’s been a big shift for ACT Pathology, transforming its lab into a 24-hour operation and adding staff to help process COVID-19 tests, all while still carrying out its usual workload. But the process of having a swab to getting your COVID-19 result has been relatively unknown until now. Sebastian Violante, 11, and ACT Pathology invited the Sunday Canberra Times to have a behind-the-scenes look at how Canberra’s front-line workers deal with suspected coronavirus cases. Sebastian is one of the 178,000 people who have been tested, with 113 positive cases and three deaths in the past 12 months. Sebastian is among Canberrans who’ve presented for testing at a government-run facility with mild respiratory illness symptoms. A sore throat and runny nose is all it takes to qualify for a coronavirus test; people who have lost their sense of smell or are experiencing a fever are also asked to come in for a test. After arriving at the Garran surge centre, which has since closed as a testing site and shifted to delivering COVID-19 vaccines, Sebastian and his mum were provided with face masks and required to sanitise their hands. Nurse Ann Halloran runs through a series of screening tests, to make sure Sebastian really does need a test. What are his symptoms? Has he been in contact with a known case of coronavirus? Ms Halloran also checks Sebastian into the system, noting his arrival and presentation. Then Sebastian is escorted through to a socially-distanced waiting area, with chairs set apart in a separate room of the pop-up hospital, built in case overflow wards were needed to treat COVID-19 patients but instead put into use as a central site in pandemic prevention. Soon, Sebastian is called through to sit in a bay where his sample will be collected. First, a registered nurse runs through a checklist of questions for Sebastian. What is your date of birth? What symptoms do you have? Do you consent to a test for COVID-19 today? Now for the unpleasant bit. A second nurse, wearing full personal protective equipment including a clear face shield, prepares Sebastian to collect a sample, using a swab at the back of his nose and his throat. It’s uncomfortable – but it’s over quickly. From there, Sebastian’s job is done. All he needs to do now is isolate until he gets his result. No leaving home, no seeing friends, no interacting with others. Mum is on hand to take him home, from a specially designated exit. Meanwhile, Sebastian’s sample is bagged and its labels checked. It’s now ready for collection. The samples are collected in humble red cooler boxes and they are transported from the site on the Garran Oval on foot directly to the hospital pathology lab over the road. Collections take place at set times throughout the day. Wearing a high-visibility vest, technical officer Himalaya Khajanchi carries the cooler and walks over the road – navigating through the pedestrians on the fringe of the busy hospital’s campus – to Building 10. After taking the lift, Mr Khajanchi drops the cooler to the pathology team tasked with logging every sample that comes in for analysis. Most of the samples come in after 1pm each day, but samples are received between 10am and 8pm each day. It’s an odd combination of laboratory and office. Sitting at computer desks wearing white coats, staff handle samples and feed the patient information provided into ACT Pathology’s computer system. Each sample is carefully tracked and labelled, so vials and samples can be tracked every step of the way. A member of staff takes the samples upstairs to the lab. Here, technical officer Erica Hu prepares Sebastian’s sample for analysis, transferring it onto the testing media and using a centrifuge to prepare it for the machine. Ms Hu loads the sample into the Panther analysis machine, which was added to the pathology lab’s arsenal of testing equipment last year. The lab runs multiple analysers to prevent any downtime, and to allow urgent tests to be streamlined. Once the need for COVID-19 testing is less urgent, the Panther machine will be used for other diagnostic tests. Sebastian’s sample is rushed into the machine to demonstrate the process, but samples would normally be processed in batches of 40 at a time. Once they have been loaded, the machine can take over. The time taken for a coronavirus test has remained steady since the beginning of the pandemic, but improvements in the administration have seen wait times for patients drop. It takes about three hours to analyse the sample. Pathologists are careful about one distinction: a negative result really means the coronavirus has not been detected in the sample, not absolute proof the person does not have COVID-19. If the analysis does not detect the coronavirus, the machine automatically sends a text message to the person. This is why people waiting for their results can receive their message in the middle of the night. The pandemic prompted a new system to integrate analysis and sending out results. In the early months, it was a full-time job for staff to enter and check data from analysed results to send out results. If the sample comes back positive, there’s no automatic text message. Laboratory staff check the machine and then prompt ACT Health to contact the person. The process of contact tracing and supporting a positive COVID-19 case would begin. Sebastian’s mum gets the text message saying the COVID-19 virus was not detected in his sample at 11.39pm, less than seven hours after his sample was collected. Most tests take longer, as Sebastian’s was expedited to demonstrate the process. Many results come back in 24 hours, but some take up to 72 hours. In the early days, Professor Kennedy said, there was already a sense the coronavirus pandemic could be bigger than the ones that had come before: SARS, MERS or Ebola. “There was just some reason we thought, ‘I think this is going to be bigger’. [We] started preparing for testing in the ACT, because we just had this feeling that we’re going to need to get these tests done more rapidly than we can if we send them to Sydney,” she said. Using a testing method published by the World Health Organisation – “Like a recipe”, Professor Kennedy said – ACT Pathology ran its first tests for COVID-19 on February 10, 2020. “We ran eight patients that day. We’re now running 500 to 1500 a day,” Prof Kennedy said. More than 170,000 negative tests have been recorded in the ACT since the pandemic began. Negative samples are kept for a month, while all positive coronavirus samples have been stored. The samples help the lab run genome sequencing, track emerging strains, and assess whether new laboratory assays are up to scratch. Professor Kennedy said it had been a long year and she was proud of the work microbiologists had done in the pandemic response. “It’s just been a massive effort. Initially with the public labs, and then also the private labs doing the bulk of the testing now across Australia. I think it’s just remarkable what we’ve actually done,” she said. Professor Kennedy is excited for the vaccination roll out and returning, hopefully, to something like Canberra had in 2019 before the bushfires and COVID-19. “You never get surprised in medicine. Something will pop up. But I think across Australia, we’ve probably come across every scenario of possible transmission events that can occur, so hopefully we won’t see too many anymore and we can concentrate on getting everyone vaccinated,” she said. While the Garran Surge Centre is no longer open for COVID-19 testing, free tests are available at the Weston Creek Walk-in Centre, the drive-through facility at Exhibition Park in Mitchell, and the Kambah drive-through testing centre on Jenke Circuit. Our journalists work hard to provide local, up-to-date news to the community. This is how you can continue to access our trusted content:
/images/transform/v1/crop/frm/35sFyBanpD896MKnAH5FRtj/2d991aa9-1278-46dd-9cb5-6e9917c40251.jpg/r0_482_5000_3307_w1200_h678_fmax.jpg
It’s the brief moment of discomfort more than 170,000 Canberrans have endured as part of the effort to keep a deadly pandemic in check.
But what happens to the swab after it’s put so far enough up your nose your eyes begin to water? COVID-19 testing has been the key component of the large-scale public-health effort to reduce the coronavirus impact in Canberra.
Canberra’s first COVID-19 test was conducted on February 10 last year. The first case was confirmed a month later on March 11. Since then, testing rates have ebbed and flowed – numbers rising to almost unmanageable peak levels after confirmed cases and then dropping to be almost non-existent when people become complacent.
Professor Karina Kennedy, ACT Pathology’s director of clinical microbiology, has overseen a year of tremendous change, battling equipment shortages and demand spikes to keep test results flowing out smoothly.
“We only had seven existing staff in that area, so we were fortunate in that the hospital and Health supported us in being able to realise that we did more staff. So we were able to quickly train up a good group of people who could actually do that role,” Professor Kennedy said.
“We wouldn’t have been able to do it with the existing staffing that we had, because it’s just such a small unit to start with.”
In a year since the first tests were completed – at a time when scientists were still scrambling globally to understand much of the virus and the potentially fatal disease it causes – Canberra’s ability to process large batches of tests each day has surged ahead.
It’s been a big shift for ACT Pathology, transforming its lab into a 24-hour operation and adding staff to help process COVID-19 tests, all while still carrying out its usual workload.
But the process of having a swab to getting your COVID-19 result has been relatively unknown until now.
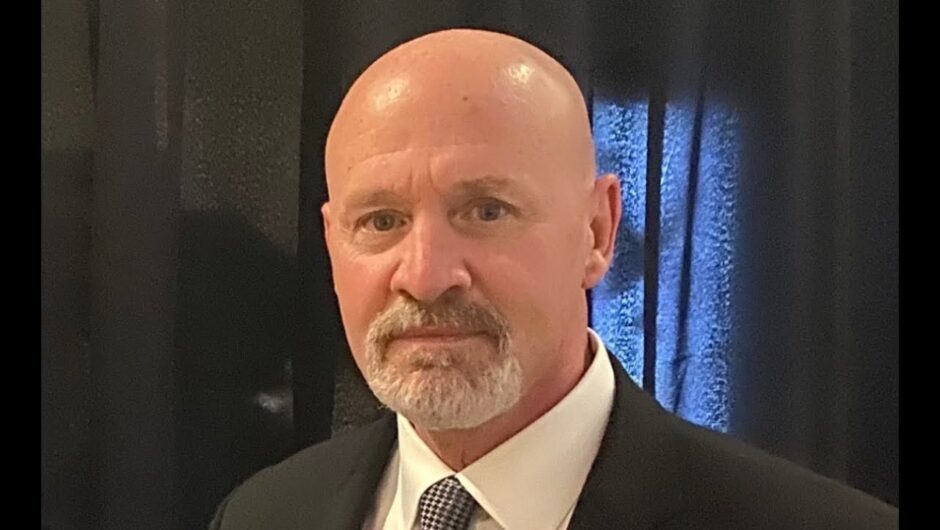
Sebastian Violante, 11, and ACT Pathology invited the Sunday Canberra Times to have a behind-the-scenes look at how Canberra’s front-line workers deal with suspected coronavirus cases. Sebastian is one of the 178,000 people who have been tested, with 113 positive cases and three deaths in the past 12 months.
Sebastian Violante arrives at the Garran Surge Centre for a COVID-19 test. The centre has since closed for testing and now is a vaccination site. Picture: Sitthixay Ditthavong
Sebastian is among Canberrans who’ve presented for testing at a government-run facility with mild respiratory illness symptoms. A sore throat and runny nose is all it takes to qualify for a coronavirus test; people who have lost their sense of smell or are experiencing a fever are also asked to come in for a test.
After arriving at the Garran surge centre, which has since closed as a testing site and shifted to delivering COVID-19 vaccines, Sebastian and his mum were provided with face masks and required to sanitise their hands.
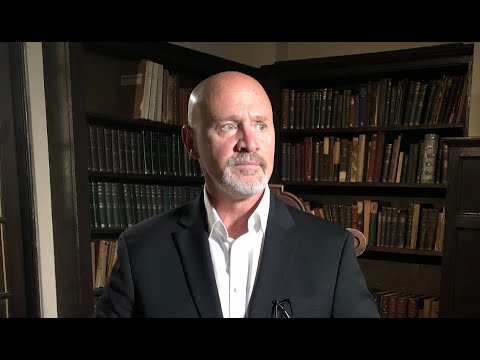
Nurse Ann Halloran runs through a series of screening tests, to make sure Sebastian really does need a test. What are his symptoms? Has he been in contact with a known case of coronavirus? Ms Halloran also checks Sebastian into the system, noting his arrival and presentation.
Sebastian Violante answers preliminary questions from registered nurse Ann Halloran before being admitted for a COVID-19 test. Picture: Sitthixay Ditthavong
Then Sebastian is escorted through to a socially-distanced waiting area, with chairs set apart in a separate room of the pop-up hospital, built in case overflow wards were needed to treat COVID-19 patients but instead put into use as a central site in pandemic prevention.
Soon, Sebastian is called through to sit in a bay where his sample will be collected.
Sebastian Violante waits to be called in for his COVID-19 test in a socially-distanced waiting area. Picture: Sitthixay Ditthavong
First, a registered nurse runs through a checklist of questions for Sebastian. What is your date of birth? What symptoms do you have? Do you consent to a test for COVID-19 today?
Now for the unpleasant bit. A second nurse, wearing full personal protective equipment including a clear face shield, prepares Sebastian to collect a sample, using a swab at the back of his nose and his throat.
It’s uncomfortable – but it’s over quickly.
Sebastian Violante has to answer a few more questions before his test. Picture: Sitthixay Ditthavong
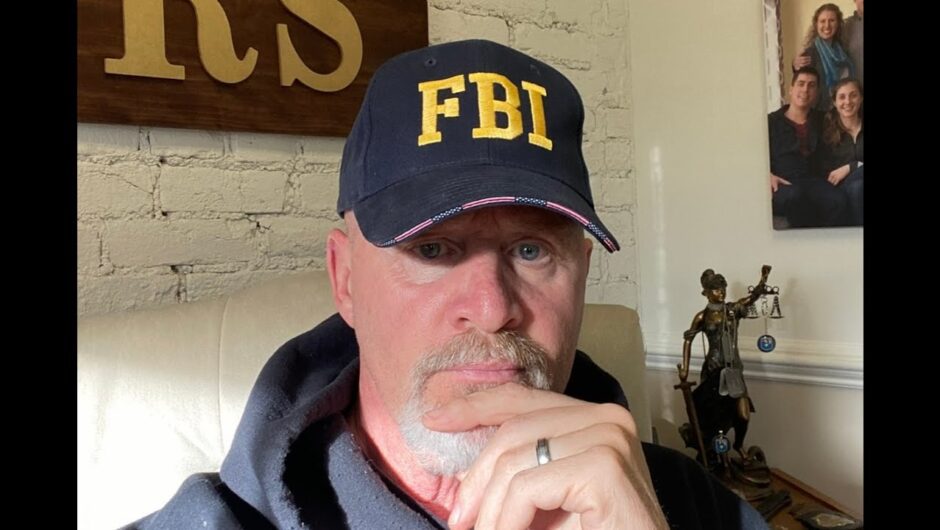
From there, Sebastian’s job is done. All he needs to do now is isolate until he gets his result. No leaving home, no seeing friends, no interacting with others. Mum is on hand to take him home, from a specially designated exit.
Meanwhile, Sebastian’s sample is bagged and its labels checked. It’s now ready for collection.
The samples are collected in humble red cooler boxes and they are transported from the site on the Garran Oval on foot directly to the hospital pathology lab over the road. Collections take place at set times throughout the day.
Sebastian Violante gets ready to have a swab taken for his COVID-19 test. Picture: Sitthixay Ditthavong
Wearing a high-visibility vest, technical officer Himalaya Khajanchi carries the cooler and walks over the road – navigating through the pedestrians on the fringe of the busy hospital’s campus – to Building 10.
After taking the lift, Mr Khajanchi drops the cooler to the pathology team tasked with logging every sample that comes in for analysis. Most of the samples come in after 1pm each day, but samples are received between 10am and 8pm each day.
It’s an odd combination of laboratory and office. Sitting at computer desks wearing white coats, staff handle samples and feed the patient information provided into ACT Pathology’s computer system.
A nurse wearing full personal protective equipment takes a saliva sample for Sebastian Violante’s COVID-19 test. Picture: Sitthixay Ditthavong
Each sample is carefully tracked and labelled, so vials and samples can be tracked every step of the way. A member of staff takes the samples upstairs to the lab.
Here, technical officer Erica Hu prepares Sebastian’s sample for analysis, transferring it onto the testing media and using a centrifuge to prepare it for the machine.
Ms Hu loads the sample into the Panther analysis machine, which was added to the pathology lab’s arsenal of testing equipment last year. The lab runs multiple analysers to prevent any downtime, and to allow urgent tests to be streamlined. Once the need for COVID-19 testing is less urgent, the Panther machine will be used for other diagnostic tests.
Once collected, the samples are stored in red coolers ready to be transported to the laboratory for analysis. Picture: Sitthixay Ditthavong
Sebastian’s sample is rushed into the machine to demonstrate the process, but samples would normally be processed in batches of 40 at a time.
Once they have been loaded, the machine can take over.
The time taken for a coronavirus test has remained steady since the beginning of the pandemic, but improvements in the administration have seen wait times for patients drop.
It takes about three hours to analyse the sample. Pathologists are careful about one distinction: a negative result really means the coronavirus has not been detected in the sample, not absolute proof the person does not have COVID-19.
COVID-19 technical officer Himalaya Khajanchi collects samples from the COVID-19 surge centre in Garran. Picture: Sitthixay Ditthavong
If the analysis does not detect the coronavirus, the machine automatically sends a text message to the person. This is why people waiting for their results can receive their message in the middle of the night.
The pandemic prompted a new system to integrate analysis and sending out results. In the early months, it was a full-time job for staff to enter and check data from analysed results to send out results.
If the sample comes back positive, there’s no automatic text message. Laboratory staff check the machine and then prompt ACT Health to contact the person. The process of contact tracing and supporting a positive COVID-19 case would begin.
Himalaya Khajanchi walks the chest of samples from the Garran testing centre to the Canberra Hospital over the road. Picture: Sitthixay Ditthavong
Sebastian’s mum gets the text message saying the COVID-19 virus was not detected in his sample at 11.39pm, less than seven hours after his sample was collected. Most tests take longer, as Sebastian’s was expedited to demonstrate the process. Many results come back in 24 hours, but some take up to 72 hours.
Technical officer Jane Astbury enters data associated with the collected samples, before the samples can be sent up for analysis. Picture: Sitthixay Ditthavong
In the early days, Professor Kennedy said, there was already a sense the coronavirus pandemic could be bigger than the ones that had come before: SARS, MERS or Ebola.
“There was just some reason we thought, ‘I think this is going to be bigger’. [We] started preparing for testing in the ACT, because we just had this feeling that we’re going to need to get these tests done more rapidly than we can if we send them to Sydney,” she said.
Using a testing method published by the World Health Organisation – “Like a recipe”, Professor Kennedy said – ACT Pathology ran its first tests for COVID-19 on February 10, 2020.
“We ran eight patients that day. We’re now running 500 to 1500 a day,” Prof Kennedy said.
More than 170,000 negative tests have been recorded in the ACT since the pandemic began.
Technical officer Erica Hu prepares the samples for testing using a centrifuge. Picture: Sitthixay Ditthavong
Negative samples are kept for a month, while all positive coronavirus samples have been stored. The samples help the lab run genome sequencing, track emerging strains, and assess whether new laboratory assays are up to scratch.
Professor Kennedy said it had been a long year and she was proud of the work microbiologists had done in the pandemic response.
“It’s just been a massive effort. Initially with the public labs, and then also the private labs doing the bulk of the testing now across Australia. I think it’s just remarkable what we’ve actually done,” she said.
Erica Hu loads the samples onto the Panther analysis machine at the ACT Pathology laboratory, the final stage of COVID-19 testing. Picture: Sitthixay Ditthavong
Professor Kennedy is excited for the vaccination roll out and returning, hopefully, to something like Canberra had in 2019 before the bushfires and COVID-19.
“You never get surprised in medicine. Something will pop up. But I think across Australia, we’ve probably come across every scenario of possible transmission events that can occur, so hopefully we won’t see too many anymore and we can concentrate on getting everyone vaccinated,” she said.
While the Garran Surge Centre is no longer open for COVID-19 testing, free tests are available at the Weston Creek Walk-in Centre, the drive-through facility at Exhibition Park in Mitchell, and the Kambah drive-through testing centre on Jenke Circuit.
Our journalists work hard to provide local, up-to-date news to the community. This is how you can continue to access our trusted content: