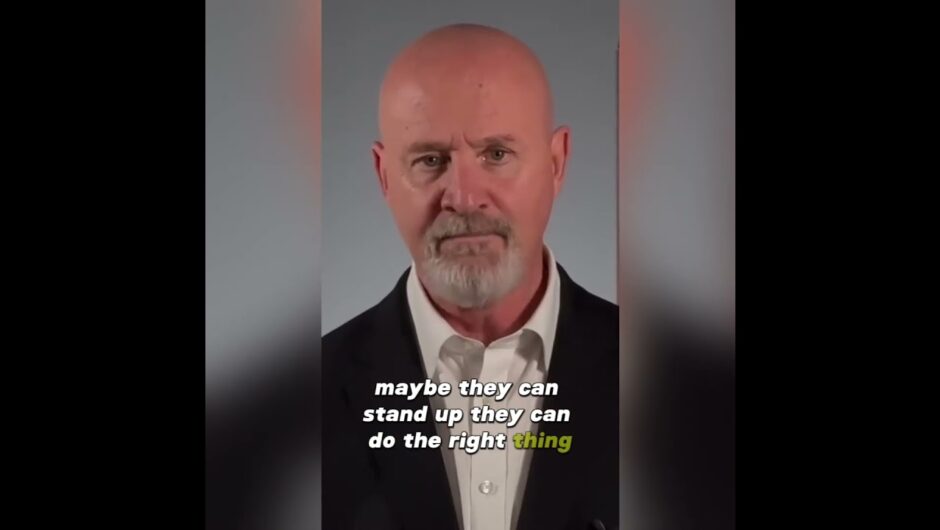
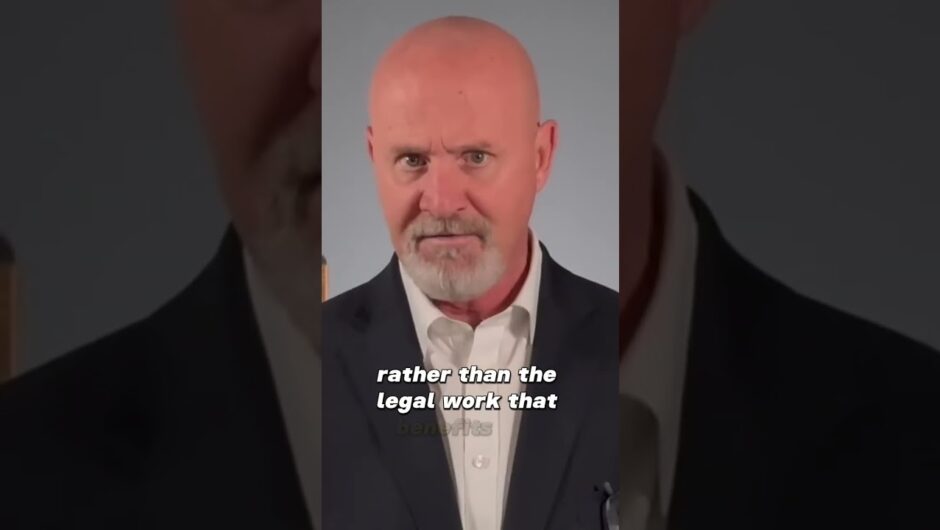
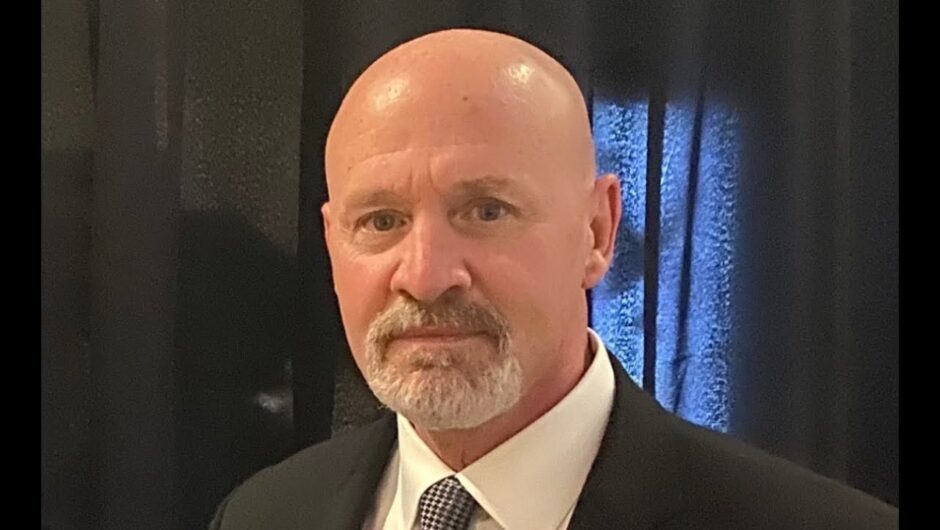
A neuro-oncologist and spinal surgeon at Greenslopes Private Hospital, in Brisbane’s south east, Koefman regularly informs patients of devastating, incurable diagnoses, dashing future hopes, dreams and aspirations. He described the moment when the light in some patients’ eyes was “unplugged’’.“It’s an extraordinary thing to tell someone,’’ Koefman said.“Patients are usually fairly well at the time and it is hard for them to comprehend that in six to 12 months they are going to be dead.“There are a handful of cases I remember the look in the person’s eyes … you can see the power plug that gives a person life and aspirations just being unplugged. There’s a sense of inevitability there and you can see the light go out of their eyes.“It’s like in nature when a deer is being chased by a lion or a leopard. The deer has a strong survival instinct and that is the most powerful instinct of all. It will run and run and run but, if the leopard catches it, at some point that deer has to surrender its survival and accept its fate.’’
Koefman, 39, who specialises in brain tumours, degenerative conditions and spinal trauma, must deliver the worst possible news to patients almost weekly, a part of his job he called “a torrid process’’.He has worked with patients of all ages and said he had particularly struggled breaking the news of incurable conditions to parents of children. “I really find that the hardest because I’m not really talking to the patient, I’m talking to the patient’s parents,’’ he said.“Just imagine caring for a child for years and years and then to be told they have x-number of months to live. It’s an extraordinarily difficult process. I have had to do that and I really struggle with that.’’Speaking exclusively to The Courier-Mail, Koefman candidly described how aspects of the job – constantly telling people bad news and bad outcomes – affected doctors’ mental health.“There are lots of pressures on doctors and they all chip away at you,’’ he said.“It’s not a surprise to have to tell a patient bad news – it’s always on the horizon to happen again – but, having said that, every single time is still a bit of a jolt.“In the moment when it is actually happening, it’s a stark reminder of the reality of the situation. It’s not an autopilot process, it’s quite a profound experience each time.“You go home and think about that. You try to fathom what that must actually feel like to be told you have a limited amount of time left.“I might think about a case for a week or a couple of weeks before I have to focus on the next case in front of me.’’
Koefman said he had various strategies to cope with his work’s heavy emotional toll – including working out at the gym once or twice daily, watching cricket and Formula One sports, and drumming in a band – but, most essentially, he regularly talked to colleagues and mentors. He has seen colleagues “crash and burn’’ without leaning on others for support.Medical oncologist Dr Margie McGrath works at Princess Alexandra Hospital and Greenslopes Private Hospital, specialising in treatment of patients with head, neck, lung and brain cancers.She works with patients on their cancer treatment and management, sometimes forging relationships with people over several years.
While not usually providing the initial diagnosis, McGrath, 46, still often informed patients their treatment options had been exhausted or that their cancer had spread.After developing ongoing relationships with patients, getting to know their partners, children, grandchildren and family situations, McGrath said breaking devastating news about their cancer often filled her with anxiety and dread.“You get very attached to people,’’ she said.“I definitely feel anxious and sometimes it’s a feeling of dread. You know what impact what your words will have on the patient and their whole family.“There are some awful cases and sometimes a big concern is what is going to happen to the kids, particularly if the patient is a single parent.“You don’t have the same conversations for every person. Each person is individual and you know which people want you to tell it straight, while some don’t want to know how long they have, others will like a hug, others not.“When you have really good relationships with patients, it is like you are sharing the news with them. You go through it with them. And, sometimes, those times are more difficult because you can feel like you are letting them down.’’
Breaking through the virtual screen
McGrath, a mother to three children, admitted the job was sometimes emotionally exhausting and she often took thoughts of patients home with her, hashing over in her mind whether there was anything more she could have done and imagining what the patient’s family was going through.“You have to stop yourself. You have to try not to feel responsible,’’ she said.“Having my kids at home, my focus goes onto what to cook for dinner, helping with homework, managing their problems, which is good. But I’m also constantly getting work related phone calls and text messages throughout the evening and night.“Watching bad television also helps me switch off, just sitting in front of it mindlessly … sometimes that is just what you need.’’McGrath also stressed the importance of talking to colleagues to share the load of heartbreak and that it was common for doctors to feel overwhelmed.“There’s just a huge emotional component to the job,’’ she said.“But it is also extremely rewarding to see the positive differences that some of our treatments can make to people’s lives. And it really is a privilege to share the ups and downs with the patients and their families.’’
You can have your cake and bake it, too
Koefman said he has become better at delivering bad news to his patients thanks to more years’ experience but also pondering life’s bigger questions about consciousness, humanity and psychology.An experience two years ago while performing an operation called an awake craniotomy – where the patient remained conscious during an operation on their brain – also took his patient interactions to a “deeper level’’. Although he had done the operation many times before, on this occasion he was struck with a “moment of wonder’’ as he watched the patient have a “conscious experience’’ on one side of the drapes, while on the other he saw the brain – a “physical thing conducting electrical impulses”.“I remember the first time I had to tell a patient they had a terminal diagnosis. At the time, I was very much a scientist and surgeon and it was pathology,’’ he said.“But I’ve become very interested in consciousness … the whole concept of being alive; what is life and what does it mean?“I began to realise the impact of my words on the patient and have a deeper understanding of what they were going through.’’
Source link