news, act-politics, act health, act mental health
Canberrans needing mental health treatment were being left with no option but to attend hospital because of a shortfall in community-based services, a mental health researcher says. While the most recent data showed the ACT government had increased mental health funding, much of it had occurred at the acute level, allowing it to increase beds at the under pressure Canberra Hospital. At the same time, funding for community-based mental health care had been on the decline. Sebastian Rosenberg, from the Centre for Mental Health Research at Australian National University, said the government would never be able to keep up with demand if it poured money primarily into acute services. “I can guarantee you if you have more beds they will fill,” he said. “You’ve just created a larger point of crisis.” In 2014-15, 24.7 per cent of all ACT spending on mental health was directed at hospitals. But in 2018-19, the last available year of data, it represented 45.7 per cent of spending. At the same time, funding for psychosocial services provided by non-government organisations fell from 18.1 per cent of total funding to 8 per cent, while community residential care funding fell from 13.4 per cent to 3.9 per cent. The number of available acute beds in the ACT during that timeframe rose from 70 to 122, as demand for hospital psychiatric services dramatically increased. Dr Rosenberg said the drop in funding had meant there were often no available government-funded services between a psychologist appointment and admission into hospital. “Rather than reinforcing old, expensive and often traumatic models of hospital-based mental health care, we need to plan now for a service system where most services are available in or from a person’s home,” he said. “We know that acute hospitalisation is both expensive and often traumatic. We know that the vast majority of ‘episodes’ include many missed opportunities to intervene earlier and provide the support necessary to diminish the severity of the impacts of mental illness.” Dr Rosenberg said much of the fall in community-based funding coincided with the rollout of the NDIS in the territory. “Like all jurisdictions, the ACT shifted a very large chunk of its psychosocial resources to the NDIS as part of its initial establishment,” he said. “Effectively, this cordoned off resources previously available to the general public to just those who were in receipt of an NDIS care package.” The Productivity Commission data showed the number of Canberrans who were discharged from a mental health ward and were subsequently readmitted within 28 days was also on the rise. “The data reveals that Canberrans increasingly have little choice but to seek their mental health care at hospital and they are more likely to require swift readmission,” Dr Rosenberg said. ACT Mental Health Minister Emma Davidson said improving community-based mental health services was a key focus of the government. “We’re about to launch the Step Up, Step Down program which is a sub-acute service that supports people to transition between services that better meet their mental health needs,” she said. “We are also increasing beds in sub-acute facilities such as the Brian Hennessy Rehabilitation Centre and continuing to work with and support community organisations who deliver services for people experiencing mild-moderate mental health concerns.” Ms Davidson said she was working closely with ACT Health and Canberra Health Service to get their advice on where the main need for mental health services in the community was. “They provide us with evidence about what’s happening on the ground and keep us connected with healthcare workers so we can continue to improve services,” she said.
/images/transform/v1/crop/frm/fdcx/doc7ct1cy0wdtl10jycwhpm.jpg/r2_258_5046_3108_w1200_h678_fmax.jpg
Canberrans needing mental health treatment were being left with no option but to attend hospital because of a shortfall in community-based services, a mental health researcher says.
While the most recent data showed the ACT government had increased mental health funding, much of it had occurred at the acute level, allowing it to increase beds at the under pressure Canberra Hospital.
At the same time, funding for community-based mental health care had been on the decline.
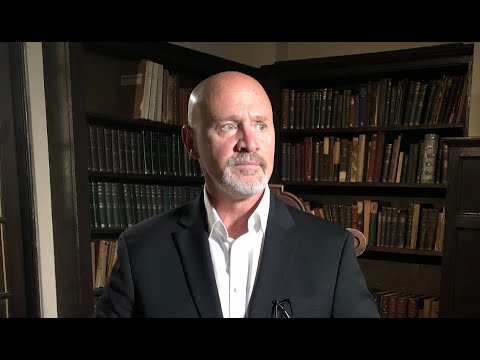
Sebastian Rosenberg, from the Centre for Mental Health Research at Australian National University, said the government would never be able to keep up with demand if it poured money primarily into acute services.
“I can guarantee you if you have more beds they will fill,” he said.
“You’ve just created a larger point of crisis.”
In 2014-15, 24.7 per cent of all ACT spending on mental health was directed at hospitals.
But in 2018-19, the last available year of data, it represented 45.7 per cent of spending.
At the same time, funding for psychosocial services provided by non-government organisations fell from 18.1 per cent of total funding to 8 per cent, while community residential care funding fell from 13.4 per cent to 3.9 per cent.
The number of available acute beds in the ACT during that timeframe rose from 70 to 122, as demand for hospital psychiatric services dramatically increased.
Dr Rosenberg said the drop in funding had meant there were often no available government-funded services between a psychologist appointment and admission into hospital.
“Rather than reinforcing old, expensive and often traumatic models of hospital-based mental health care, we need to plan now for a service system where most services are available in or from a person’s home,” he said.
“We know that acute hospitalisation is both expensive and often traumatic. We know that the vast majority of ‘episodes’ include many missed opportunities to intervene earlier and provide the support necessary to diminish the severity of the impacts of mental illness.”
Dr Rosenberg said much of the fall in community-based funding coincided with the rollout of the NDIS in the territory.
“Like all jurisdictions, the ACT shifted a very large chunk of its psychosocial resources to the NDIS as part of its initial establishment,” he said.
“Effectively, this cordoned off resources previously available to the general public to just those who were in receipt of an NDIS care package.”
The Productivity Commission data showed the number of Canberrans who were discharged from a mental health ward and were subsequently readmitted within 28 days was also on the rise.
“The data reveals that Canberrans increasingly have little choice but to seek their mental health care at hospital and they are more likely to require swift readmission,” Dr Rosenberg said.
ACT Mental Health Minister Emma Davidson said improving community-based mental health services was a key focus of the government.
“We’re about to launch the Step Up, Step Down program which is a sub-acute service that supports people to transition between services that better meet their mental health needs,” she said.
“We are also increasing beds in sub-acute facilities such as the Brian Hennessy Rehabilitation Centre and continuing to work with and support community organisations who deliver services for people experiencing mild-moderate mental health concerns.”
Ms Davidson said she was working closely with ACT Health and Canberra Health Service to get their advice on where the main need for mental health services in the community was.
“They provide us with evidence about what’s happening on the ground and keep us connected with healthcare workers so we can continue to improve services,” she said.