Based on early studies, Pfizer has said it does not expect a significant reduction in the effectiveness of its vaccine. The company says it can quickly adjust its vaccine if necessary.
However, that is based on laboratory studies, not human data. And all four vaccines use different technologies but have an identical core component – a piece of the virus’ spike protein they try to generate an immune response to.
Nurse Novita Sirait (ight) gives a shot of the COVID-19 vaccine to a colleague at a community health centre in Medan, North Sumatra, Indonesia.Credit:AP Photo/Binsar Bakkara
Pfizer’s vaccine was approved for use in Australia in January, and 53.8 million doses of AstraZeneca’s vaccine have been bought and will be distributed over coming months.
The federal government did not respond to questions about this story by Monday’s deadline.
The South African variant of the virus has been picked up eight times in Australia.
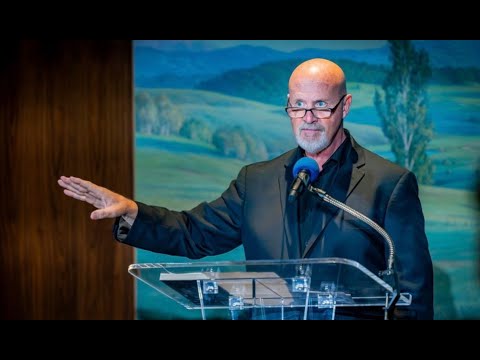
“It is hard to say for sure, but you would think there is the potential they would also be reduced,” said Associate Professor Corey Smith, head of translational and human immunology at the QIMR Berghofer Medical Research Institute.
He said the results suggested the virus could mutate in ways that made antibodies and vaccines less effective. “But I don’t think that’s a real surprise,” he said. “Viruses always mutate.”
The South African variant, known as N501Y.V2, has several mutations that in lab tests appear to change the shape of the virus’ spike in a way that reduces the ability of some antibodies generated from infection with the original Wuhan variant of COVID-19 from binding.
That raises concerns about reinfection, and about how well COVID-19 vaccines based on the original variant will protect against the South African variant.
Professor David Tscharke, head of the department of immunology and infectious diseases at the Australian National University, said it was always likely that “we will have to chase variants by changing our vaccines”.
However, he said it was not clear cut that AstraZeneca and Pfizer’s vaccines faced the same problems as Novavax and Johnson & Johnson.
“You might guess that but the extent of that is going to be varied,” he said. “Although they have the same antigens, they are presented in a different way.”
Virus-killing T cells also played a role in immunity, he said, and they might allow Pfizer and AstraZeneca’s jabs to still offer strong protection against the variant.
Early lab evidence suggested Pfizer’s vaccine would be less effective against the South African variant, but would still cover the virus.
But those studies were carried out using “pseudoviruses” – viruses manipulated to look like N501Y.V2 – and were done on cells in a lab. Such studies do not always translate to humans.
Novavax and Johnson & Johnson are the first vaccine developers to report human data on the variants.
Novavax’s trial of more than 4400 patients in South Africa reported efficacy of 49.4 per cent (excluding HIV-positive patients, efficacy rose to 60 per cent). Nearly all the cases of infection among vaccinated subjects were from the South African variant.
Johnson & Johnson’s trial of 6576 people in South Africa reported efficacy of 57 per cent; 95 per cent of infections in people vaccinated were from the South African variant.
These trials were small and the results were preliminary, experts said. South Africa also presents a unique environment to test vaccines: a runaway epidemic means people may be exposed to unusually high levels of virus.
Loading
But even with all that in mind, said Associate Professor Stuart Turville, a virologist at the Kirby Institute, “the data early on, looks like the edge has been taken off by the South African variant”.
“What we’re seeing in the real world is this thing has the potential to take the edge off vaccines. Which may mean we need to update the formulation.”
The experts emphasised it was important to wait for real-world data from Pfizer and AstraZeneca. It may be the vaccines’ different designs work better against the variant.
These vaccines also stimulate T-cell immunity – although it is not clear what role that plays in protection from COVID-19.
And even a vaccine with reduced effectiveness was much better than no vaccine at all.
“To put this into context, we’re still getting significant protection,” said Professor Tscharke. “We could be living in a world where all these vaccines were giving numbers like that all around the world – and we would still be pretty happy.”
Examine newsletter
Science and health explained and analysed with a rigorous focus on the evidence. Examine is a weekly newsletter by science reporter Liam Mannix. Coming soon, sign up now.
Liam is The Age and Sydney Morning Herald’s science reporter
Most Viewed in National
Loading